

Intramedullary spinal cord abscesses are infrequently encountered in everyday neurosurgical practice. Hart reported the earliest documented spinal cord abscess in 1830. Since then, fewer than 100 cases have been reported in the medical literature. With modern antibiotics and neurosurgical techniques, even smaller numbers of these infections are expected to be encountered in the future. Since abscesses may occur anywhere along the spinal axis, anatomy varies with location involved. The most common location for an intramedullary abscess is the posterior thoracic spinal cord.
Since the original publication of this article, several other case reports have been published that discuss intramedullary spinal cord abscesses.[1, 2, 3, 4] These case reports, while detailing several unusual presentations of patients with intramedullary spinal cord abscesses, add little to the core concepts promulgated in the original article. Patients with intramedullary spinal cord abscesses present with neurological findings related to the level of spinal cord involvement; MRI with gadolinium is still the procedure of choice for early diagnosis; and successful outcomes depend upon early diagnosis, aggressive surgical treatment, and appropriate antibiotic treatment following surgery. Even when these guidelines are followed, 70% of patients are left with neurological sequelae.
The presumptive diagnosis of intramedullary abscess requires prompt definitive diagnosis. This of course necessitates demonstration of an infection with subsequent identification of that organism. Therefore, a laminectomy to diagnose and culture the organism is usually required.
See the image below.
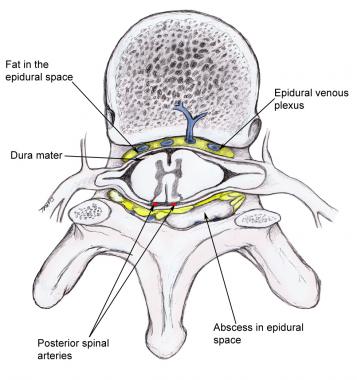 Abscess that compresses the spinal cord and its vasculature.
Next
Abscess that compresses the spinal cord and its vasculature.
Next
Spinal cord abscesses arise in spinal cord parenchyma and can be solitary or multiple, contiguous or isolated, and chronic or acute, depending upon the organism and individual patient. As may be expected, solitary lesions are more common and most likely appear in the thoracic cord. Holocord abscesses have been reported in approximately 5 patients. Some authors divide these abscesses into primary and secondary, depending on the source of infection. Abscesses are considered primary when no other infection source can be found. Secondary abscesses arise from another infection site, either distant from or contiguous to the spinal cord, most commonly from the lung, spine, heart valves, and genitourinary system. Intramedullary spinal cord abscesses most commonly arise from a secondary source such as the cardiopulmonary system or from a source in close proximity to the cord such as the mediastinum. These classifications rarely affect treatment or patient outcome.
Spinal cord abscesses occur more frequently in males than females with a peak incidence in the first and third decades of life. Too few cases have been reported to define any racial predilection. Patients with a history of intravenous drug abuse are at particularly high risk, as are other immunocompromised patients such as those with HIV, diabetes, or multiple organ failure.
The most common organisms cultured from spinal cord abscesses include Staphylococcus and Streptococcus species, followed by gram-negative organisms. Mixed flora abscesses are also encountered.
Other unusual organisms have been reported, including Actinomyces, Listeria, Proteus, Pseudomonas, Histoplasma capsulatum, and the tapeworm Sparganum.
In 1899, Hoche demonstrated that abscesses may occur in areas of infarction, thus explaining the common incidence of septic spread to the lower half of the thoracic cord.
The Batson plexus (the confluence of epidural veins in the spinal canal) may contribute to the origin of an abscess by allowing organisms to lodge and thus develop in the spinal cord and its surrounding parenchyma.
Postoperative intramedullary spinal cord abscess due to Mycoplasma hominis has been reported after a neurosurgical procedure.[5] Intramedullary Aspergillus abscess has also been reported.[6]
Spinal cord abscesses have many of the same characteristics of abscesses in other locations. Blood vessel involvement surrounded by an area of infection characterizes hematogenous spread. Areas of softening and early abscess formation characterize subacute infections (1-2 wk duration), whereas a classic abscess wall of fibrotic gliosis surrounding necrotic purulent material characterizes chronic infections. However, spinal cord abscesses do not destroy fiber tracts. Instead, the abscess displaces fiber tracts and spreads along axonal pathways.[7]
As with most neurological diseases, signs and symptoms depend upon the abscess location and duration. In an acute presentation, symptoms of infection (eg, fever, chills, back pain, malaise) are common. Neurological symptoms and signs include weakness, paresthesia, dysesthesia, bladder and bowel incontinence, and acute paraplegia. The neurological signs and symptoms are dependent upon the location in the spinal cord of the abscess with the most common location for an intramedullary abscess is the thoracic spinal cord. Clinical symptoms are similar to those of patients with epidural abscesses, but percussion tenderness is not noted.
In more chronic cases, signs and symptoms mimic those of an intramedullary tumor, and neurological symptoms predominate over those of a systemic infection. The neurological progression is gradual. A high degree of awareness is necessary to diagnose chronic spinal cord abscess; in contrast, acute abscesses are generally encountered in extremely ill patients presenting with acute onset of back pain.[8]
The outcome is generally good with appropriate use of antibiotics and surgical treatment. However, the abscess location determines the residual neurologic deficits. The patient's degree of sepsis ultimately establishes overall mortality. With the advent of modern antibiotics and lower surgical mortality, most abscesses are treated successfully. With steroids and more timely localization through MRI, neurologic deficits can be reduced.
However, patients may be affected by devastating neurologic sequelae and may succumb to this disease. Overall mortality rates vary from 10-20%. Moreover, approximately 70% of patients demonstrate residual neurological sequelae following appropriate treatment. Importantly, a significant percentage of patients have recurrence of the abscess. Consequently, repeat MRIs are essential in patients' long-term and follow-up care.
For excellent patient education resources, visit eMedicineHealth's Infections Center and Brain and Nervous System Center. Also, see eMedicineHealth's patient education articles Brain Infection and Antibiotics.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved