

In 1920, Scheuermann first described the clinical findings of structural thoracic kyphosis. However, it was not until 1964 that Sorensen defined the radiographic findings in Scheuermann kyphosis.[1] He described the defining characteristic of anterior wedging of 5° or more in at least three adjacent vertebral bodies. This helped to objectify and differentiate Scheuermann kyphosis from postural round back deformity.
Scheuermann thoracic kyphosis is a structural deformity of the thoracic spine, defined by anterior wedging of at least 5° of three or more adjacent thoracic vertebral bodies (see the image below).
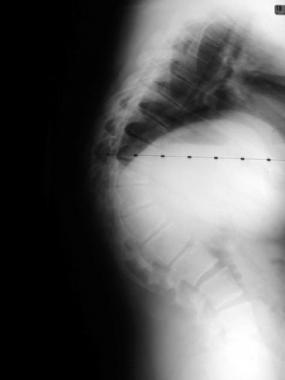 Preoperative lateral radiograph of patient with 85° thoracic deformity secondary to Scheuermann kyphosis.
Preoperative lateral radiograph of patient with 85° thoracic deformity secondary to Scheuermann kyphosis.
Further radiographic findings include Schmorl nodes and endplate narrowing. Although the etiology of Scheuermann kyphosis (Scheuermann disease) remains unknown, the natural history and treatment indications are well described.
Both adolescents and adults can develop symptoms associated with Scheuermann kyphosis. Adolescents typically develop a progressive cosmetic deformity, which first brings them in for medical attention, whereas adults with long-standing deformity typically develop pain as an indication for treatment.
Bracing has been demonstrated to be an effective treatment modality for the adolescent with a progressive deformity, whereas pain often responds to nonoperative care, including physical therapy and anti-inflammatories in both adolescents and adults. In patients with a progressive deformity, refractory pain, or neurologic deficit, surgical correction may be indicated.
Guidelines for treatment, surgical options and techniques, and complications are discussed in this article.[2]
NextHistorically, surgical care of Scheuermann kyphosis (Scheuermann disease) has shadowed surgical care of idiopathic scoliosis. The role of surgical care for adolescent kyphosis was debated in the sparse literature before 1960. In 1962, Paul Harrington introduced the Harrington rod to augment the surgical correction of scoliosis. In 1965, Moe presented his nonoperative and operative results from a posterior approach in the treatment of adolescent kyphosis. Postoperative curve progression and a high pseudoarthrosis rate complicated the posterior-only approach.[3]
Combined anterior and posterior surgical approaches for Scheuermann kyphosis were first popularized in the 1970s. These techniques increased fusion rates and correction and remain the foundation of current surgical approaches. Subsequent innovations included simultaneous thoracoscopic anterior release with postinstrumented fusion.
Differentiating normal thoracic kyphosis from abnormal thoracic kyphosis (Scheuermann kyphosis, or Scheuermann disease) is somewhat problematic. Normal thoracic kyphosis is actually dynamic throughout life and typically increases.
Fon et al measured thoracic kyphosis in children younger than 10 years and in adolescents aged 19 years and younger.[4] In those younger than 10 years, he found that the average kyphosis was 20.00° with a standard deviation (SD) of 7.85 for boys and 23.87° with an SD of 6.67 for girls. Shelton et al have reported on the diagnosis and management of kyphosis in adolescents.[5, 6]
In adolescents, the kyphosis had increased to an average of 25.11° with an SD of 8.16 in boys and 26.00° with an SD of 7.43 in girls. Females, on average, have slightly greater kyphosis in the thoracic spine throughout life. This difference between males and females increases further when they are older than 40 years.
In women aged 50-59 years, the average kyphosis measured 40.71° with an SD of 9.88°, whereas men in the same age group had an average thoracic kyphosis of 33.00° with an SD of 6.46.
For purposes of definition, any degree of kyphosis of more than 40° should be deemed abnormal. Additionally, any degree of kyphosis at the thoracolumbar junction or in the lumbar area of the spine should be considered abnormal.
The prevalence of Scheuermann kyphosis (Scheuermann disease) is estimated to be 4-8% of the general population. Sorensen reported a prevalence of 0.4-8.3%.[1] Scoles et al reported on 1384 cadaveric specimens and noted a 7.4% prevalence of Scheuermann kyphosis.[7]
Although the prevalence of Scheuermann kyphosis is generally accepted as being essentially equal in males and females, there is some debate regarding this finding in the literature. Bradford et al reported a female-to-male ratio of 2:1 for Scheuermann kyphosis.[8, 9] Meanwhile, Murray et al reported the exact opposite finding, with a 2.1:1 male-to-female ratio.[10] In Sorenson's work, 58% of the patients were male, and 42% were female.[1]
The proximate cause of Scheuermann kyphosis (Scheuermann disease) has not yet been determined. Scheuermann initially hypothesized that avascular necrosis of the ring apophysis led to premature cessation of growth anteriorly and subsequent wedging of the vertebral body. Schmorl later postulated that traumatic herniations of disk material through the vertebral endplates led to subsequent loss of disk height and anterior vertebral wedging. Both of these theories were disproved later.
Halal reported on five families in which Scheuermann kyphosis appeared to transfer in an autosomal-dominant mode of inheritance.[11] To date, the genetic marker has not been determined.
Skogland[12] and Ascani[13] proposed other theories that Scheuermann kyphosis is based on a genetic inheritance.[12] Skogland reported on 62 females aged 9-18 years, whose mean height was an average of 2.5 standard deviations (SDs) above average. Of these 62 females, 18 had thoracic kyphosis of more than 40°, with 11 additional participants having vertebral anomalies consistent with Scheuermann kyphosis.
Ascani also presented work demonstrating a similar correlation between Scheuermann kyphosis and height. He also demonstrated increased levels of growth hormone.[13]
Damborg et al found a heritability of 0.74 in Scheuermann's disease, with a lower threshold in men than women.[14]
A study by Hershkovich et al suggested that height and body mass index (BMI) are associated with the risk and severity of spinal deformities in adolescents.[15] The study, which included 103,249 males and females aged 17 years who had been diagnosed with some degree of kyphosis or scoliosis, found that in underweight males and females, spinal deformities were significantly more common and were more likely to be severe. Greater height was also associated with increased risk and greater severity of spinal deformities in males and females.
Mechanical factors have been postulated as a cause for Scheuermann kyphosis.[16] Scheuermann initially noted a higher incidence of kyphosis in industrial workers and found that hyperextension bracing is helpful in curbing the progression of Scheuermann kyphosis, which would support a mechanical etiology. However, the radiographic and histologic changes of Scheuermann kyphosis have not yet been demonstrated to be in fact secondary or primary in the development of Scheuermann kyphosis.
Although the etiology of Scheuermann kyphosis (Scheuermann disease) is not yet understood, the histologic and pathologic findings are well described. Radiographically, the presence of three
adjacent wedged vertebral bodies of at least 5° each is pathognomonic for Scheuermann kyphosis. Anatomic findings include a thickened anterior longitudinal ligament (ALL) with narrowed intervertebral disks. The vertebral bodies are wedged, and traumatic disk herniations through the endplates are consistent findings.
The ratio of collagen to proteoglycans in the matrix of the endplate in patients with Scheuermann kyphosis has been described as low in comparison with that in patients without the condition. This relative decrease in collagen has been hypothesized to lead to an alteration in the ossification of the endplate and, thus, to altered vertebral body growth.
Finally, osteoporosis has been postulated to have a role in the pathology and etiology of Scheuermann kyphosis. Bradford reported on 12 patients with Scheuermann kyphosis who were prospectively studied with an extensive osteoporosis workup, including an iliac crest biopsy.[17] Some of the patients with Scheuermann kyphosis were demonstrated to have a mild form of osteoporosis, although the cause and effect of this finding in terms of developing Scheuermann kyphosis was not made.
A follow-up study by Gilsanz reported 20 adolescent patients aged 12-18 years with Scheuermann kyphosis who demonstrated no evidence of osteoporosis as measured by quantitative computed tomography (CT).[18]
Bradford, however, had surmised that the osteoporosis was transient and somehow led to altered vertebral growth and, thus, to the formation of Scheuermann kyphosis.[17] This etiologic hypothesis remains a subject of debate.
Scheuermann kyphosis (Scheuermann disease) may be entirely asymptomatic. However, patients with Scheuermann kyphosis who present for medical attention generally have problems that fall under one of the following five categories:
When present, pain should be highly concordant with the location of the spinal deformity in Scheuermann kyphosis. Pain may be present in either adolescence or adulthood, though it is a more typical presenting complaint in adults. Characteristically, the pain is located just distal to the apex of the deformity and then radiates laterally in a paraspinal pattern. The pain also is activity related and often abates with rest.
Address atypical pain, particularly in adolescents, with further diagnostic studies. Adults with pain often have low back pain, secondary to hyperlordosis below the Scheuermann kyphosis and subsequent degenerative disk disease and facet arthropathy, or the pain may be due to associated spondylolisthesis. Note that pain is the presenting complaint in 20-60% of patients with Scheuermann kyphosis.
Progressive deformity in the absence of radiographic conformation is difficult to document, though the history of the deformity should be queried. Patients and, particularly, family members often note a deformity that worsens over time. Clothes fit differently, shoulders appear more rounded, and it may appear that the length of the arms is increasing out of proportion to the rest of the body. Radiographic confirmation of progressive deformities is ideal.
If progression of the curve is documented, particularly in an adolescent, consider more aggressive treatment options.
Neurologic risk related to Scheuermann kyphosis is quite rare, but when it is present, it typically mandates a surgical approach. A short-segment severe deformity generally is considered to be a curve that is at highest risk secondary to the cord being draped over the deformity with anterior compression.
Lonstein et al demonstrated an average kyphosis of 95° in patients who presented with neurologic compromise.[19] However, Ryan and Taylor presented three patients with Scheuermann kyphosis and neurologic compromise with an average kyphosis of only 54°.[20]
Spinal stenosis of the lumbar spine below the deformity may lead to neurogenic claudication in the adult patient, and although it is not directly attributable to Scheuermann kyphosis, it may complicate the clinical picture.
Congenital thoracic stenosis has been reported in association with Scheuermann kyphosis and may lead to myelopathy or intraoperative complications during correction of the deformity.
Cardiopulmonary compromise as a presenting complaint for patients with Scheuermann kyphosis is quite rare. Restrictive lung disease has been documented by Murray et al,[10] yet this was in curves of more than 100°, with the apex of the curve located in the upper thoracic region. Sorensen reported earlier that chest wall abnormalities in patients with Scheuermann kyphosis had no negative effect on cardiopulmonary function.[1]
Finally, cosmetic issues should not be underestimated in the evaluation of a patient with Scheuermann kyphosis. Address these concerns specifically and aggressively with the individual patient, because they ultimately prove to be the driving force behind the patient's decision process. When cosmesis is the isolated indication for treatment, particularly for surgical care, exercise caution.
After the history has been well documented, a physical examination completes the initial clinical evaluation. Scheuermann kyphosis must be differentiated from postural kyphosis. On physical examination, this difference is made on hyperextension. Patients with Scheuermann kyphosis, even adolescents, demonstrate a structural deformity that only partially corrects on hyperextension. Patients with postural kyphosis, by contrast, have flexible deformities.
Forward flexion delineates the deformity quite well, with shorter angulated curves presenting as an A-frame deformity. Overall, sagittal alignment usually is maintained, secondary to compensatory hyperlordosis of both the cervical and lumbar spine. Perform a lower extremity neurologic evaluation, paying particular attention to any signs of upper motor neuron compromise. Findings typically are normal.[21]
Indications for treatment in patients with Scheuermann kyphosis (Scheuermann disease) typically mirror the presenting complaints — namely pain, progressive deformity, neurologic compromise, cardiopulmonary issues, or cosmesis. Tailor the recommended treatment to the individual, and base treatment not only on the severity of symptoms but also on the correlation between symptoms and the deformity.
Additionally, in making decisions regarding treatment options, the physician must understand the natural history of Scheuermann kyphosis. Generally, the degree of clinical problems mirrors the magnitude of the deformity. Therefore, expect patients with mild deformities to have mild clinical symptoms.
Murray et al reported the natural history and long-term follow-up of patients with Scheuermann kyphosis,[10] monitoring 67 patients with a mean kyphotic angle of 71° for an average of 32 years. Patients with Scheuermann kyphosis had more intense back pain (typically localized to the thoracic spine) and overall had less demanding jobs and less mobility in the thoracic spine. However, in both these patients and the age-matched controls, levels of education, absenteeism from work, physical activity, medication use, and social interactions were found to be similar.
Other authors have presented a higher prevalence of problems in patients with Scheuermann kyphosis. Bradford reported a 50% incidence of severe thoracic back pain in his patients with thoracic deformities and a higher incidence of back pain in patients with thoracolumbar deformities.[8] Lowe et al reported a high correlation between low back pain and severe thoracic deformity.[22]
Despite varying opinions on the natural history of Scheuermann kyphosis, there does appear to be a subset of adult patients who develop refractory pain. Knowing that a subset of adolescents who have progressive curves eventually develop painful deformities in adulthood affects treatment decisions earlier in life. The additional psychosocial effect of the deformity also must be considered. Neurologic and cardiopulmonary risks are exceedingly low; when encountered, they must be addressed on an individual basis.
The anatomy relevant to patients with Scheuermann kyphosis (Scheuermann disease) depends on the planned treatment. Surgical care for patients with Scheuermann kyphosis can be provided via a posterior, an anterior, or a combined anterior-posterior approach (see Intraoperative details).
Contraindications to treatment in patients with Scheuermann kyphosis (Scheuermann disease) are relative. With any treatment option, benefits must be weighed against risks for each individual patient. The magnitude of surgical intervention must be considered in the light of the perceived benefit and risk. Surgical care of patients with severe thoracic deformities is a large undertaking, and medical comorbidities must be considered.
Neurologic compromise as a result of surgical intervention is the most catastrophic complication compatible with life that exists in treatment of patients with Scheuermann kyphosis. The incidence of neurologic compromise increases in revision spinal surgery, particularly with revision anterior approaches. Previous history of pulmonary compromise is a relative contraindication for an anterior approach. This should include previous history of empyema, which may complicate the surgical approach.
Although no absolute contraindications exist to the surgical care of patients with Scheuermann kyphosis, the magnitude of the clinical problem and pervasiveness of the symptoms in the patient's life must be matched by the radiographic deformity and the surgeon's personal expertise.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved