

The first description of rupture of the rotator cuff tendon was by Smith in 1834.[1, 2] With history, degenerative changes of the rotator cuff have been better characterized by Duplay,[3] Von Meyer,[4] Codman,[5] and Neer.[6] The exact mechanisms leading to the degeneration of the rotator cuff, however, are still being debated.
Shoulder pain is the third most common cause of musculoskeletal disorders (MSDs), after low back and neck pain. Although considered a benign condition, according to a study on the long-term outcome of rotator cuff tendinitis, 61% of the patients were still symptomatic at 18 months, despite receiving what was considered sufficient conservative treatment. Moreover, 26% of patients rated their symptoms as severe. MSDs are the primary disabling conditions of working adults. The prevalence of rotator cuff tendinitis has been found to be as high as 18% in certain workers who performed heavy manual labor.
Webster and Snook estimated that the mean compensation cost per case of upper extremity work-related MSDs was $8070 in 1993; the total US compensable cost for upper extremity, work-related MSDs was $563 million in the 1993 workforce. The compensable cost is limited to the medical expenses and indemnity costs (lost wages). When other expenses (eg, full lost wages, lost production, cost of recruiting and training replacement workers, cost of rehabilitating the affected workers) are considered, the total cost to the national economy becomes much greater.[7]
The impact of rotator cuff disease on quality of life is even more difficult to assess than its cost. Further studies using valid methods such as the Medical Outcomes Study (MOS) 36-item short-form health survey (SF-36), which measure the impact of the disorder on general health, should help assess this issue.
NextThe rotator cuff is composed of four muscles—the subscapularis, supraspinatus, infraspinatus, and teres minor—and their musculotendinous attachments (see the image below).
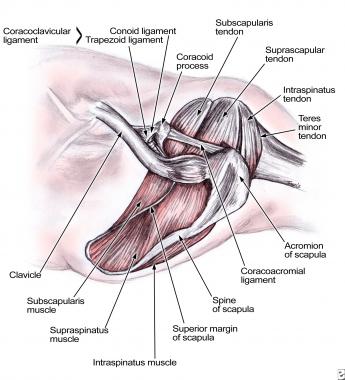 Rotator cuff anatomy.
Rotator cuff anatomy.
The subscapularis is innervated by the subscapular nerve and originates on the scapula. It inserts on the lesser tuberosity of the humerus. The supraspinatus and the infraspinatus are both innervated by the suprascapular nerve, originate in the scapula, and insert on the greater tuberosity. The teres minor is innervated by the axillary nerve, originates on the scapula, and inserts on the greater tuberosity. The subacromial space lies underneath the acromion, the coracoid process, the acromioclavicular joint, and the coracoacromial ligament. A bursa in the subacromial space provides lubrication for the rotator cuff.[8, 9]
Understanding the functional anatomy of the rotator cuff assists in understanding its disorders. The rotator cuff is the dynamic stabilizer of the glenohumeral joint. The static stabilizers are the capsule and the labrum complex, including the glenohumeral ligaments. Although the rotator cuff muscles generate torque, they also depress the humeral head. The deltoid abducts the shoulder. Without an intact rotator cuff, particularly during the first 60° of humeral elevation, the unopposed deltoid would cause cephalad migration of the humeral head, with resulting subacromial impingement.
Rotator cuff pathology can result from extrinsic (outside) or intrinsic (from within) factors. Extrinsic examples include a traumatic tear in tendons from a fall or accident. Overuse injuries from repetitive lifting, pushing, pulling, or throwing are also extrinsic in nature. Intrinsic factors include poor blood supply, normal attrition or degeneration with aging, and calcific invasion of tendons.[8, 10, 11, 12, 13, 14]
Rotator cuff tendinitis is the term used to describe irritation of tendons either from excessive pressure on the acromion or, less commonly, from intrinsic tendon pathology. Irritation of the adjacent bursa is known as subdeltoid or subacromial bursitis. Repetitive overhead activities resulting in irritation of tendons and bursae from repeated contact with the undersurface of the acromion is termed impingement syndrome.
Rotator cuff dysfunction is typically a continuum of pathology ranging from tendinitis and bursitis, to partial tearing, to a complete tearing in one or more of the tendons. Although the earlier stages may resolve with conservative care, actual tearing of the tendon can be more problematic. These tears most commonly occur at the tenoperiosteal (tendon-to-bone) junction. Because this area has a relatively poor blood supply, injury to the tendon at this location is very unlikely to actually heal.
Additionally, the constant resting tension in the muscle-tendon unit, or muscle tone, pulls any detached fibers away from the bone, preventing their reattachment. Finally, joint fluid from within the shoulder may seep into the tear gap and prevent the normal healing processes from occurring.
Possible causes of rotator cuff pathology are as follows:
Shoulder pain is the third most common cause of MSDs, after low back pain and cervical pain. Estimates of the cumulative annual incidence of shoulder disorders range from 7% to 25% in the Western general population. The annual incidence is estimated at 10 cases per 1000 population, peaking at 25 cases per 1000 population in persons aged 42-46 years.
In persons aged 70 years or older, 21% of persons have shoulder symptoms, most of which were attributed to the rotator cuff. In cadaver studies, the rate of full thickness tears varies from 18-26%. The rate of partial thickness tears ranges from 32% to 37% after age 40 years. Before age 40 years, tears are rare. In magnetic resonance imaging (MRI) studies, tears have been observed in 34% of asymptomatic individuals of any age. After age 60 years, 26% of patients have partial thickness tears, and 28% demonstrate full-thickness tears.
No known racial variation associated with rotator cuff disease is cited in the literature. In one study, a predominance of male patients (66%) seeking consultation for rotator disease is reported, but in other studies, the male-to-female ratio is 1:1. Rotator cuff disease is more common after age 40 years. The average age of onset is estimated at 55 years.
An estimated 4% of cuff ruptures develop a cuff arthropathy. Various authors report the success rate of conservative treatment to be 33-90%, with longer recovery time required in older patients. Surgery results in better function regardless of the patient's age.
Piasecki et al found that arthroscopic-revision rotator cuff repair may be a reasonable treatment option even after previous open repairs, providing improved pain relief and shoulder function. In the 54 patients, studied, the American Shoulder and Elbow Surgeons scores improved from 43.8 ± 5.7 to 68.1 ± 7.2, and the Simple Shoulder Test improved from 3.56 ± 0.8 to 7.5 ± 1.1. Visual analog pain scale scores improved from 5.17 ± 0.8 to 2.75 ± 0.8 (P = .03), and forward elevation increased from 121.0º ± 12.3º to 136º ± 11.8º. The authors noted that female patients and those who had undergone more than one ipsilateral shoulder surgery had poorer results.[15]
In a systematic review of the published literature, Nho et al compared single-row (SR) with double-row (DR) suture anchor fixation in arthroscopic rotator cuff repair. The authors found no clinical differences between the SR and DR suture anchor repair techniques. They concluded that the data in the published literature do not support the use of DR suture anchor fixation to improve clinical outcome, although they noted that there are some studies reporting that DR suture anchor fixation may improve tendon healing.[16]
A meta-analysis that included three randomized controlled studies and two controlled clinical cohort studies compared outcomes between SR and DR rotator cuff repair. The results found that while the DR technique significantly increased operative time, it provided greater external rotation, improved tendon healing, and decreased recurrence rate. However, no significant differences were found between the two techniques with regard to shoulder function, muscle strength, forward flexion, internal rotation, patient satisfaction, or return to work.[17]
One study analyzed the structural and functional outcomes after arthroscopic rotator cuff repair between SR, DR, and combined DR/suture-bridge techniques. After an average follow-up of 38.5 months, the data noted that repair with combined DR/suture-bridge technique resulted in an overall decreased retear rate, especially for large and massive tears. This combined technique proved to be an effective option for arthroscopic rotator cuff repair.[18]
Schofer et al, in a prospective, randomized, controlled study, compared high-energy extracorporeal shock-wave therapy (ESWT) with low-energy ESWT in the treatment of rotator cuff tendinopathy. Patients in the high-energy group received 6000 impulses of ED+ 0.78 mJ/mm2 in three sessions, and those in the low-energy group received 6000 impulses of ED+ 0.33 mJ/mm2. An increase in function and a reduction of pain were found in both groups. Although the improvement in Constant score was greater in the high-energy group, statistical analysis showed no significant difference between the two groups regarding Constant score, pain reduction, and subjective improvement after 12 weeks and after 1-year follow-up.[19]
Drake et al reviewed the use of reverse total shoulder arthroplasty (RTSA) in patients with rotator cuff disease.[20] The authors found that modern RTSA designs restore deltoid tension and a functional fulcrum to the rotator cuff-deficient shoulder, allowing recovery of active shoulder elevation and restoring function. Contraindications to RTSA include severely impaired deltoid function, an isolated supraspinatus tear, and the presence of full active shoulder elevation with a massive rotator cuff tear and arthritis. The authors concluded that for properly selected patients with symptomatic and disabling rotator cuff deficiency, RTSA can yield life-changing improvements in pain, motion, function, and patient satisfaction.[20]
Wellmann et al concluded that for patients with symptomatic and disabling rotator cuff deficiency, RTSA can result in a significant reduction in pain and improvements in motion and function.[21]
Using propensity-matching methods, one study compared the outcomes of patients with pseudoparalytic large-to-massive tears with those of nonpseudoparalytic tears after rotator cuff repair and whether the presence of pseudoparalysis negatively affected the outcome. The study observed evidence of recovery from pseudoparalysis in a large portion of the study group; similar outcomes were noted in postoperative function and cuff healing, whether pseudoparalysis was present or not. Considering the possible complications from treatment with RTSA, the study authors suggest that rotator cuff repair should be the first-line treatment option for large-to-massive tears.[22]
Data from one study noted that the failure rate after arthroscopic rotator cuff repair was significantly higher in patients with lower bone mineral density, a higher grade of fatty infiltration of the infraspinatus, and greater amount of retraction.[23]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved