

A claw toe is a lesser toe with dorsiflexion of the proximal phalanx on the lesser metatarsophalangeal (MTP) joint and concurrent flexion of the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints (see the images below).
 Claw toe.
Claw toe.
 Plastic model of claw toe.
Plastic model of claw toe.
The term claw toe is most likely derived from the affected toe's similarity in appearance to the claw of an animal or talon of a bird (see the image below). The talon typically curves upward before it makes a descending C-shaped curve.
 Claw toe is named for its similarity to an eagle claw or talon.
Claw toe is named for its similarity to an eagle claw or talon.
Claw toe is distinguished from hammer toe by the combination of dorsiflexion of the MTP joint and plantarflexion of the DIP joint in the former condition (see the image below). In contrast, a hammer toe may have some hyperextension at the MTP joint or some flexion at the DIP joint, but it does not have both concurrently. Typically, the DIP joint is extended in a hammer toe.
 Claw toe. Plastic model of hammer toe.
Claw toe. Plastic model of hammer toe.
Hammer toe is differentiated from curly toe, which has combined plantarflexion of all three joints (see the first image below), as well as from mallet toe, which has a neutral position of the MTP and PIP joints and flexion at the DIP joint (see the second and third images below). Clawing often affects multiple toes (see the fourth image below).[1, 2, 3, 4]
 Claw toe. Curly toe.
Claw toe. Curly toe.
 Claw toe. Mallet toes 3 and 4.
Claw toe. Mallet toes 3 and 4.
 Claw toe. Mallet toe.
Claw toe. Mallet toe.
 Multiple claw toes.
Multiple claw toes.
Table 1 contains descriptions of lesser toe deformities.
Table 1. Lesser Toe Deformities (Open Table in a new window)
Deformity MTP Joint PIP Joint DIP Joint Hammer toe Dorsiflexed* or neutral Plantar flexed Neutral, hyperextended, or plantar flexed* Claw toe Dorsiflexed Plantar flexed Plantar flexed Mallet toe Neutral Neutral Plantar flexed Curly toe Neutral or plantar flexed Plantar flexedThe extensor tendon crosses and is held over the MTP joint by an aponeurotic band of fibrous tissue. Although it does not insert into the proximal phalanx, it is able to dorsiflex the proximal phalanx of the MTP joint through this aponeurotic band, which goes around the MTP joint and is inserted onto the plantar plate (see the image below).
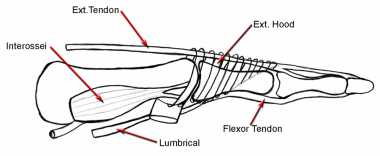 Claw toe. Extensor tendon connecting with extensor hood.
Claw toe. Extensor tendon connecting with extensor hood.
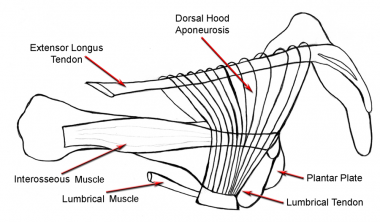
The extensor tendon splits into three parts over the proximal phalanx. The central slip attaches itself to the dorsal aspect of the base of the middle phalanx. The medial and lateral slips rejoin distally to insert on the dorsal aspect of the base of the distal phalanx (see the image below). The extensor tendon is only capable of extending the PIP and DIP joints when the MTP joint is in neutral flexion; otherwise, this is accomplished by the intrinsic musculature.[5, 6, 7, 8]
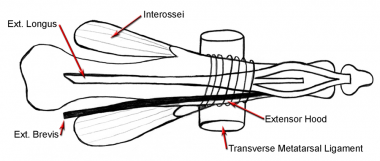 Claw toe. Extensor tendon splits into 3 parts distally.
Claw toe. Extensor tendon splits into 3 parts distally.
The intrinsics are made of the lumbricals, which are strong extenders of the PIP and DIP joints by virtue of their attachment onto the extensor sling and the interossei. Interossei are weak extensors of the interphalangeal joints because so few fibers reach the extensor sling. Furthermore, when the MTP joint is hyperextended, the lumbrical power in extending the PIP and DIP joints is reduced because of a mechanical disadvantage.
The flexor digitorum longus (FDL) tendon inserts into the plantar aspect of the distal phalanx, and the flexor digitorum brevis (FDB) inserts onto the middle phalanx. Thus, no major antagonist to dorsiflexion of the proximal phalanx is present. Hence, when the proximal phalanx dorsiflexes, static tightening of the flexors occurs, which subsequently flexes the PIP and DIP joints. Stabilization of the lesser MTP joint comes from the static restraint of the plantar plate and the collateral ligaments.
The collateral ligaments have been reported as the primary stabilizers of the lesser MTP joint. The two sets of collateral ligaments both emanate from the lateral metatarsal head. The phalangeal collateral ligament inserts into the proximal phalanx, and the accessory collateral ligament inserts onto the plantar plate. The plantar plate is attached from the base of the proximal phalanx to an origin on the metatarsal head, just proximal to the plantar articular cartilage.
When the collateral ligaments and plantar plate lose resiliency or are stretched through repetitive dorsal directing forces on the proximal phalanx from ground reactive forces, the proximal phalanx dorsiflexes. Without a strong plantar flexor attached to the proximal phalanx, the proximal phalanx remains in dorsiflexion, and the PIP and DIP joints subsequently flex (see the image below).
 Claw toe. Plantar plate stretches out, and proximal phalanx is dorsiflexed.
Claw toe. Plantar plate stretches out, and proximal phalanx is dorsiflexed.
When the flexed position of the PIP and DIP joints remains constant, the collateral ligaments fibrose along the sides of the PIP and DIP joints, and the position of their joints becomes fixed. When this occurs, the claw toe deformity becomes rigid, whereas previously it was considered flexible. This separation of flexible and rigid most often occurs at the PIP joint.
Claw toe deformity results from altered anatomy or neurologic deficit that leads to an imbalance between the intrinsic and extrinsic musculature to the toes.[9, 10]
The prevalence of claw and hammer toe deformities is in the range of 2-20%, gradually increasing with advancing age. Accordingly, claw toe is most often seen in patients in the seventh and eighth decades of life. Women are affected four to five times more than men are. Little is mentioned in the literature regarding these deformities in non-shoe-wearing populations.[11, 12, 13, 14]
Most people have no underlying disease responsible for the claw toe deformity, but it can occur in association with neuromuscular diseases, such as multiple sclerosis, Friedreich ataxia, Charcot-Marie-Tooth disease, cerebral palsy, mild dysplasia, stroke, and lumbar nerve root impingement. Metabolic diseases, such as diabetes and inflammatory arthropathies (eg, rheumatoid arthritis, psoriasis), can also be accompanied by claw toe deformity.
The experiences of other authors indicate that complete correction of the toe is necessary to achieve the best result. Of course, this presumes careful attention to detail and a toe with normal vascularity.
Taylor[15] and Pyper,[16] via transfer of both the long and short flexor to the extensor hood without bony resection, achieved only 72% and 51% good results, respectively. Pyper also noted that with soft-tissue procedures alone, the deformity recurred and results were somewhat unpredictable. Therefore, Frank and Johnson[17] and McCluskey et al[18] recommended PIP resection along with soft-tissue procedures to realign the toe.
Barbari and Brevig[19] reviewed 31 patients who had surgery on multiple toes. These authors concluded that the best cosmetic results were achieved in younger patients, and they noted that active or passive motion in the interphalangeal joints was present in 60% of these cases. Of course, restriction in range of motion is an intended outcome of the procedure. Patients must be aware that in most instances, they will sacrifice prehensile action of the toe for less pain, will have better shoe-wearing capabilities, and, ideally, will have an improved cosmetic result.
Specific disease entities seem to fare similarly; Cyphers and Feiwell[20] reported 60% good results in patients with myelomeningocele.
A prospective multicenter observational study of 117 patients requiring PIP joint realignment who underwent placement of angled intramedullary implants found that implantation resulted in a high rate of fusion and a good outcome.[21] None of the patients with incomplete joint fusion who had a stable joint with no pain required reoperation.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved