

Tarsal coalition (see the images below) is a condition in which two or more bones in the midfoot or hindfoot are joined. First described in the literature by Buffon in 1796 and subsequently described in greater detail by Cruveilhier and others,[1, 2, 3, 4, 5, 6, 7, 8] it is known to have been present in the human gene pool for a long time.[9]
 Plain radiograph (Slomann view) showing typical appearance of calcaneonavicular coalition.
Plain radiograph (Slomann view) showing typical appearance of calcaneonavicular coalition.
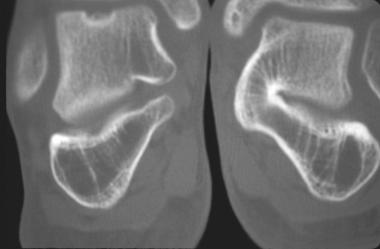 CT scan appearance of talocalcaneal coalition.
CT scan appearance of talocalcaneal coalition.
Tarsal coalitions are relatively rare. Their true incidence is unknown, because most are asymptomatic. The most common types of tarsal coalitions are those between the calcaneus and either the talus (talocalcaneal coalitions) or the navicular bones (calcaneonavicular coalitions). More than half are bilateral. Patients with this congenital condition usually present during late childhood or adolescence,[10] but presentations in adulthood have been reported.
Tarsal coalition usually presents as recurrent sprains and pain in the midfoot and has been associated with peroneal spastic flatfoot, fixed flatfoot, and other abnormalities of the foot. Radiographic evaluation has been revolutionized by the use of computed tomography (CT). Early treatment usually involves conservative modalities, including immobilization; surgical intervention includes resection of the coalition or arthrodesis of degenerated painful joints.[11, 12]
For patient education resources, see Ankle Sprain and Sprains and Strains.
NextThe normal motion of the subtalar joint during walking involves both rotation and gliding. The axis of motion of the subtalar joint is defined as a line deviated 42º from the horizontal surface and 16º medially or internally rotated from a line extending from the center of the calcaneus to a point between the first and second metatarsals.
During stance phase, the subtalar joint rotates from a position of 4º external-valgus to 6º internal-varus. This motion compensates for the horizontal external rotation of the tibia during this phase. When the internal rotation is restricted by the coalition, the tarsal joints have to compensate, with flattening of the foot and loss of longitudinal arch and a valgus appearance in the horizontal plane. This leads to an adaptive shortening of the peroneal tendons, reactive peroneal spasm, and so-called peroneal spastic flatfoot. Prolonged restriction of motion eventually may lead to posterior facet arthrosis of the subtalar joint.
Another motion of the subtalar joint lost is the gliding motion demonstrated during foot dorsiflexion. Cineradiographic studies have demonstrated a hinge motion instead, with widening at the plantar aspect of the midtarsal joints, narrowing at the dorsal surfaces, and overriding of the navicular on the talar head at maximum dorsiflexion. The traction effect of the later motion on the ligaments and capsule of the talonavicular joint is thought to be the genesis of the talar beaking seen in many radiographs of tarsal coalition.
The pain symptoms associated with tarsal coalitions may therefore be attributed to ligament sprain, peroneal muscle spasm, sinus tarsi irritation, subtalar joint irritation, and arthritic changes. The variability of the symptoms in different patients may be due to the variability of subtalar restriction of the different coalitions. The specific but different ages of presentation of different coalitions would then be due to the different ages at which coalitions ossify and thus restrict subtalar motion.
Pfitzner first proposed that the coalitions were the result of incorporation of accessory ossicles into the adjacent normal tarsal bones. This theory received some support from various authors, including Slomann, Badgley,[2] and Harris and Beath.[3] Leboucq first proposed in 1890 that the failure of segmentation of primitive mesenchyme was the cause of tarsal coalitions. His theory was supported by Solger (1890), Dwight (1907), Trolle (1948), and Jack (1954).[13]
In 1955, Harris found evidence of mesenchymal coalitions in fetal cadavers, conclusively proving Leboucq's theory. Through the work of Leonard, Wray, Herndon, and others, it is believed today that tarsal coalition is inherited in an autosomal dominant fashion with high penetrance.
The incidence of talocalcaneal coalitions in the general population is thought by most authors in the literature to be approximately 1%. Various authors have credited Pfitzner with the first incidence study but quote different percentages, ranging from 1.5-6% for the overall incidence of tarsal coalitions to 2.9% for calcaneonavicular coalitions.
Harris and Beath found 74 cases in 3600 consecutive prospective army recruits examined.[3] Rankin and Baker found 24 cases in approximately 60,000 basic trainees at Fort Dix from 1971 to 1972 (0.4%),[14] whereas Vaughn and Segal found 28 coalitions in 2000 cases of painful feet.[15] Shands and Wentz found an incidence of 0.9% in cases of painful flat feet in a pediatric clinic.[16] Leonard found that 39% of relatives of patients with symptomatic coalitions had asymptomatic coalitions.[17] Snyder et al found that 91 of 223 (63%) young patients with ankle sprains had radiographic findings suggestive of tarsal coalitions.[18]
In an evaluation of 2982 complete skeletons collected from 1910 through 1940, Cooperman et al found that 26 of them had calcaneonavicular coalitions (incidence of 1.2%).[19] Leonard found that all of the 76% of the first-degree relatives who had radiographic evidence of tarsal coalitions were asymptomatic.[17] This would suggest that the actual incidence in the population may be higher than was previously thought.
In terms of the distribution of types, Stormont and Peterson found in a review of the literature that 48.1% of the tarsal coalitions presented were talocalcaneal and 43.6% were calcaneonavicular. In their own series, the distribution was 53% calcaneonavicular and 37% talocalcaneal. The literature overall mentions a bilaterality rate of 22-60% in talocalcaneal coalitions and 40-68% in calcaneonavicular coalitions, with most being just over 50%.[20]
Sex ratios vary, with male-to-female ratios ranging from 1:1 to 4:1. No statistical difference in racial distributions has been found.
Nonoperative treatment of patients with symptomatic tarsal coalitions has not been uniformly successful. Accordingly, most long-term studies have focused on outcomes following surgical treatment. Proper patient selection is a prerequisite for optimal results.
Patients with extensive or multiple coalitions typically undergo fusion procedures, and those with less extensive or isolated coalitions undergo resection and soft-tissue interposition of their coalitions. Talar beaking must be critically evaluated but is not necessarily a contraindication for tarsal coalition resection. The vast majority of calcaneonavicular coalitions can be resected with the expectation of successful long-term results. Resection of symptomatic talocalcaneal coalitions yields optimal results when the coalition involves no more than about one third of the total joint surface.
Skwara et al assessed the foot loading characteristics and foot function in 10 patients (15 feet) who underwent surgical correction for tarsal coalition. In 12 feet, calcaneonavicular coalition was present; in three, talocalcaneal. Overall, the clinical results were fair regarding improvement of pain, range of motion, and walking distance. The American Orthopaedic Foot and Ankle Society (AOFAS) scores were fair as well (mean, 78.1) at follow-up. Gait analysis revealed alterations in kinematic and kinetic parameters for the operated foot, and pedobarographic analysis showed altered loadings for heel and forefoot.[21]
Khoshbin et al used an administrative database to follow up a cohort of patients who had undergone surgical resection of tarsal coalition with the aim of determining the rates and risk factors for subsequent resection or arthrodesis.[22] Their study cohort consisted of 304 patients (aged ≥8 years; average, 24.2 years) treated between July 1994 and August 2009. Patients with nonidiopathic coalitions were excluded. Of the 304 patients, 26 (8.6%) underwent subsequent resection, and 16 (5.3%) experienced mid- or hindfoot arthrodesis.
According to this study, the need for future fusion was more likely only if the primary resection had been performed at an academic hospital or if the patient had undergone concomitant arthrodesis at primary resection of the coalition.[22] The incidence of reoperation after primary tarsal coalition resection was low. More than 85% of the patients had not required an additional operative intervention an average of 9 years after the initial resection. The investigators suggested that primary treatment of tarsal coalition with resection and concomitant arthrodesis increases the risk of requiring a second fusion in the future.
Mahan et al evaluated patient-reported data on functional outcome after tarsal coalition resection in children and adolescents.[23] In addition to assessing medium-term (>2 years) outcomes, they compared outcomes of calcaneonavicular coalitions with those of talocalcaneal coalitions. In 73% of their patients, activities were not limited by pain. No significant differences in outcome were noted between patients treated for calcaneonavicular coalitions and those treated for talocalcaneal coalitions.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved