

In 1876, Thomas Morton first described interdigital nerve compression.[1] Morton theorized that the nerve was being compressed between the metatarsal heads. Surgical procedures have historically been aimed either at directly dealing with the pathologic nerve or at altering the local biomechanical environment in which the nerve exists. The evolution of surgical care for Morton neuroma has resulted in some basic principles and goals, which are the foundation for the current surgical options. There is an increased body of literature that elaborates on many aspects of this seemingly simple problem.
The image below depicts Morton neuroma.
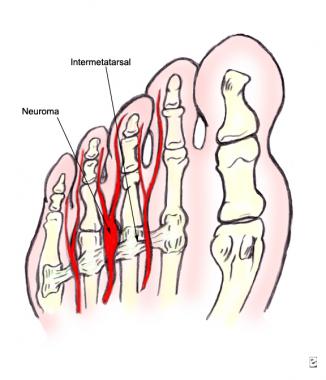 Plantar view showing the relationships between the metatarsal heads, the intermetatarsal ligament, and the neuroma.
Next
Plantar view showing the relationships between the metatarsal heads, the intermetatarsal ligament, and the neuroma.
Next
Interdigital neuritis is a mechanically induced nerve irritation due to intrinsic and extrinsic biomechanical factors that results in a combination of pain, paresthesias, and numbness in the forefoot. A greater understanding of forefoot anatomy and biomechanics has created an environment to further delineate the pathophysiology of interdigital neuroma.
Morton neuromas are more common in women, with a female-to-male ratio of 4:1. They tend to occur in the fifth decade of life and frequently are exacerbated by constrictive footwear.[2] Symptoms are typically unilateral, with the third interspace most often involved followed by the second and the fourth interspaces.[2] Simultaneous neuromas occurring in the same foot are uncommon.[3]
See Pathophysiology.
The term neuroma may be a misnomer for the condition. Morton neuroma may be best described as a clinical syndrome stemming from a constellation of factors related to the local anatomy and the forces applied on the forefoot with ambulation and shoe wear.[4] Interestingly, it is not uncommon for the histopathology to be interpreted as relatively normal, even in light of classic preoperative findings and dramatic postoperative results. Clearly, the histopathology is not that of a typical neuroma,[2] but some or all of the following may be observed:
Anatomic studies have revealed a wealth of information and helped to resolve some misconceptions regarding the etiology of this disease. The intermetatarsal space is narrower in the second and third interspaces than in the first and fourth interspaces, which correlates with the clinical presentation pattern.[5] The composition of the tarsometatarsal articulation allows relative hypermobility between the second and third metatarsals, which contributes to mechanical irritation of the nerve.
Narrow toe-box footwear can exacerbate the compression between the metatarsal heads, and hyperextension of the toes in high-heeled shoes tethers the nerve beneath the ligament and may expose it to more biomechanical stresses with gait.[2] Less commonly, metatarsophalangeal (MTP) joint pathology, inflamed bursa, or lipomas can create compression at the level of the common digital nerve.
Patients typically present with pain and paresthesias localized to one interspace of the forefoot with radiation to the involved toes. The symptoms may wax and wane over many years and are exacerbated with compressive shoewear. Relief is common when the shoes are removed and the area is massaged.[6]
A provocative examination, as shown below, involves manually compressing the forefoot and simultaneously palpating the affected web space between the fingers of the other hand. The compression may result in the Mulder sign, which is a painful and palpable click that reproduces the symptoms.[7]
 This image demonstrates the key provocative physical examination maneuver: simultaneous forefoot compression coupled with intermetatarsal space compression.
This image demonstrates the key provocative physical examination maneuver: simultaneous forefoot compression coupled with intermetatarsal space compression.
The indication for surgery is significant pain or dysfunction that is not tolerated by the patient and that fails to respond to conservative management.
In addition to the discussion above, key anatomic concepts must be considered when choosing the appropriate surgical treatment of an interdigital neuroma. The medial plantar nerve has 4 digital branches that begin at the medial aspect of the great toe and then form the common digital nerves of the first, second, and third web spaces. The lateral plantar nerve supplies the fourth web space and, in 27% of patients, contributes to the third web space. This increased thickness of the third digital nerve was hypothesized to predispose it to mechanical irritation; however, studies have shown no correlation between those patients with this anatomic variant and those with symptoms of Morton neuroma.
The common digital nerves lie plantar to the intermetatarsal ligament and give off small branches to the plantar skin approximately 1-2 cm proximal to the bifurcation of the nerve. These branches also must be resected at the time of surgery because they may prevent nerve stump retraction after neurectomy and lead to a recurrent neuroma.[1]
Once the diagnosis is made and conservative management has failed, few contraindications to surgical intervention exist. Local soft-tissue factors, such as infections or vascular insufficiency, are likely to be the only absolute contraindications. Patient psychosocial issues may be relative contraindications and must be addressed prior to surgical procedures of any kind.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved