

Most pelvic fractures are stable and occur with a low-energy mechanism of injury. The evaluation and treatment of these fractures are described in Pelvic Fractures. This article focuses on unstable pelvic fractures, which are usually caused by high-energy injuries.
The most common high-energy mechanism of injury is a motor vehicle accident. Patients who sustain these injuries not only have the osseous injury but also often have concomitant life-threatening injuries. Younger people are more likely to be involved in these accidents.[1] Early death after these injuries is usually due to hemorrhage, multiple organ system failure, or sepsis.[2] These unstable high-energy pelvic fractures require a multidisciplinary approach to treatment.
Before 1950, the treatment of pelvic fractures posed significant problems for orthopedic surgeons. Since 1950, however, significant progress has been made in understanding and treating these difficult fractures. The advent of clinically and anatomically significant classification systems has greatly increased the understanding of these injuries.
In 1948, Holdsworth reported on 27 patients with untreated sacroiliac (SI) dislocations and found that only half were able to return to work, with all 27 experiencing residual low back pain.[3] In his 1966 report on 65 patients with double vertical fractures of the pelvis, Räf noted a worse outcome when SI dislocation was present.[4] In the same report, Räf noted a high incidence of nerve injury with posterior fractures through the sacrum.
In 1972, Slatis and Huittinen reported on the late sequelae of unstable pelvic fractures, noting significant problems with pelvic obliquity, impaired gait, disabling low back pain, and signs of persistent lumbosacral plexus damage in 46% of their patients.[5] They concluded that although conservative treatment of pelvic fractures of moderate severity afforded good results, conservative treatment of severe pelvic fractures had significant shortcomings.
In 1988, Tile reported on 248 patients with pelvic ring injuries.[6] He noted that stable pelvic injuries resulted in few long-term problems. In contrast, vertically unstable injuries resulted in many problems, with 60% of patients having residual pain.
Over the past few decades, significant advances in the treatment of pelvic fractures have been made. In 1989, Matta published his techniques for operative fixation of pelvic fractures.[7] Routt has popularized percutaneous methods of fixation.[8]
The improved techniques for open reduction and internal fixation (ORIF), as well as the percutaneous fixation techniques developed, have aided greatly in the treatment of these fractures. Because of the relatively recent use of these treatments, the reporting of more long-term results of treatment is essential. These studies will direct the future treatment of unstable pelvic fractures.
Continued improvements in the multidisciplinary treatment of patients with such injuries will be crucial to further decreasing the high morbidity and mortality associated with these severe injuries.
NextA firm knowledge of pelvic anatomy is critical for understanding fracture patterns and determining treatment goals.
The three bones that compose the pelvic ring are the sacrum and the two innominate bones. Each innominate bone is formed from the fusion of three ossification centers (ie, ilium, ischium, and pubis) that join at the triradiate cartilage of the acetabulum. The innominate bones join the sacrum posteriorly at the sacroiliac joints and anteriorly at the pubic symphysis.
The posterior SI ligaments run from the sacrum to the posterior iliac spines and are the strongest ligaments in the body. The sacrotuberous ligaments consist of a strong band that runs from the posterolateral sacrum and dorsal aspect of the posterior iliac spine to the ischial tuberosity. The sacrotuberous ligaments and the posterior SI ligaments maintain the vertical stability of the pelvis.
The sacrospinous ligaments run from the lateral edge of the sacrum and coccyx, separate the greater and lesser sciatic notches, and insert on the ischial spine. The iliolumbar ligaments run from the L4 and L5 transverse process to the posterior iliac crest to provide stability between the spine and the pelvis.
An understanding of the location of major nerves and vessels in relation to the bony anatomy is particularly important in view of the development of percutaneous techniques. The sciatic nerve is formed by the roots from the lumbosacral plexus (L4, L5, S1, S2, S3) and exits the pelvis deep to the piriformis. The lumbosacral trunk is formed by the anterior rami of L4 and L5 and crosses the anterior sacral ala and the SI joint.
Fractures of the sacral ala or dislocations of the SI joints are most likely to injure the lumbosacral trunk. The L5 nerve root exits below the L5 transverse process and crosses the sacral ala 2 cm medial to the SI joint and may be injured during the anterior approach to the SI joint.
Pelvic fractures are frequently associated with large amounts of blood loss. The internal iliac artery (hypogastric artery) is the most important vascular structure in pelvic trauma. The anterior division consists of the inferior gluteal artery, the internal pudendal artery, the obturator artery, the inferior vesicular artery, and the middle rectal artery. The posterior division consists of the superior gluteal artery, iliolumbar artery, and lateral sacral artery.
The superior gluteal artery is the largest branch of the internal iliac artery. It courses along the SI joint and exits through the greater sciatic notch superior to the piriformis. This artery supplies the gluteus medius, the gluteus minimus, and the tensor fasciae latae. The superior gluteal artery is the most commonly injured artery in pelvic fractures.
Most bleeding after pelvic fractures results from venous injury. The pelvic viscera lie on a large thin-walled venous plexus that drains into the internal iliac vein. Massive bleeding may result from disruption of this venous plexus. Other neurovascular structures that lie in close proximity to the bony pelvis may be damaged when a pelvic fracture occurs.
The close relation between the urogenital tract and the bony pelvis results in a high incidence of urinary tract injuries. Bladder rupture, diagnosed by means of cystography (see the image below), and posterior urethral injuries are the most common injuries.
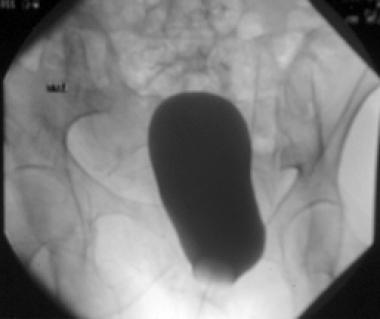 Normal bladder.
Normal bladder.
Signs of bladder injury include inability to void despite a full bladder, blood at the urethral meatus, a high-riding or abnormally mobile prostate, and an elevated bladder. Retrograde urethrography should be performed to exclude urethral injury before insertion of a Foley catheter if an anterior pelvic disruption is present or any sign of urethral injury exists (see the image below).
 Urethral injury.
Urethral injury.
Anatomic differences between males and females result in a higher incidence of urethral injuries in males. The male urethra may be divided into three sections: the prostatic portion, the membranous portion, and the bulbous portion. The bulbous urethra, located inferior to the urogenital diaphragm, is the most common site of injury. In contrast, the female urethra is short, not rigidly fixed to the pubis or pelvic floor, more mobile, and less susceptible to injury from shear forces.
If the urethra is ruptured, retrograde urethrography dye extravasates into the perineum. Impotence may occur in 25-47% of male patients with urethral rupture. Impotence is likely secondary to damage of parasympathetic nerves (S2-4). Note that the absence of meatal blood or a high-riding prostate does not exclude a urethral injury.
Bladder injuries may result from bony spicules caused by pubic rami fractures, from blunt force that causes rupture, or from shearing injuries. The superior and upper posterior portions of the bladder are covered by peritoneum. The remainder of the bladder is extraperitoneal and covered with loose areolar tissue.
Intraperitoneal ruptures usually require operative repair, whereas extraperitoneal ruptures are managed nonoperatively unless laparotomy is being performed. Extraperitoneal bladder ruptures are typically managed with suprapubic catheter drainage and broad-spectrum antibiotics. Cystography is performed before catheter removal to verify healing. About 87% of ruptures heal within 10 days, and virtually all ruptures heal within 3 weeks.
The two most commonly used classification systems are those of Tile[9, 10] and of Young and Burgess.[11, 12] These classifications help the orthopedic surgeon evaluate the stability of the pelvic injury and determine the appropriate treatment.
Tile proposed a classification into three types along a continuum of stability, as follows[9, 10]
Young and Burgess proposed a classification system based on Tile's classification. In their classification, however, they determined the injury pattern in relation to four different mechanisms of injury, as follows:
These four types of injury have been found to correlate with the resuscitation needs of the patient.[11, 12]
APC injury results from an anteriorly directed force applied directly to the pelvis or indirectly via the lower extremities (see the image below). The result is an external rotation force on the innominate bones and an open-book type injury.
 Anterior-posterior compression (APC) pelvic fracture.
Anterior-posterior compression (APC) pelvic fracture.
APC injury may be further classified into the following three subtypes, which delineate the severity of the injury by quantifying the amount of ligamentous damage present with radiographs:
LC injuries result from lateral impact of innominate bone, with internal rotation of the pelvis toward the midline. The sacrotuberous, sacrospinous, and internal iliac vessels are shortened rather than stretched. The injury sustained to the anterior ring in these injuries is not critical to the weightbearing function of the pelvis. Because of this, LC injuries are further classified into three subtypes according to the nature of the injury to the posterior ring, as follows:
A VS injury results in vertical translation of the hemipelvis (see the image below). The typical mechanism for this injury involves a fall from a height and landing on an extended limb. Anteriorly, the injury usually involves the pubic symphysis, but fractures through the pubic rami are not uncommon. Posteriorly, the force is directed through the SI joint, causing a complete disruption of this joint.
 Vertical shear (VS) fracture pattern.
Vertical shear (VS) fracture pattern.
CM injuries have features of at least two of the above-mentioned categories. The most common variety is the combination of LC and VS injuries.
A comparison of the Tile and Young-Burgess classifications systems carried out by Osterhoff et al did not identify any clinical relevant differences between the two with respect to their ability to predict mortality, transfusion or infusion requirement, or concomitant injuries.[14]
Discussion of pelvic fractures is not complete without mentioning sacral fractures. Denis classified these fractures according to their zone of injury, as follows[15] :
 Denis zone II sacral fracture.
Denis zone II sacral fracture.
High-energy injuries that result in pelvic ring disruption are more likely to be accompanied by severe injuries to the central nervous system (CNS), abdomen, and chest. These are often the results of motor vehicle accidents. The changes made in passenger restraints and an increased frequency of high-velocity motor vehicle trauma have led to a steady increase in the number of pelvic ring injuries observed and treated at trauma centers across the country.
With the institution of advanced trauma life support (ATLS) protocols, the treatment of patients with polytrauma has been associated with significant decreases in mortality. The reported range for mortality associated with pelvic ring fractures is 9-20%. The mortality among hemodynamically unstable patients has been reported to be 50%, whereas hemodynamically stable patients have a mortality of 10%.[16, 17, 18]
Young and Burgess[11] described different pelvic injury patterns observed with varying mechanisms of injury. With side-impact compression, lateral impaction injuries are observed in the pelvic ring. In head-on type collisions, an anteroposteriorly directed force results in opening of the pelvic ring and an external rotation force on the innominate bones. Combinations of these mechanisms may also occur.
Pelvic fractures account for 1-3% of all skeletal fractures and 2% of orthopedic hospital admissions. The frequency of pelvic fractures occurs in a bimodal pattern, with peaks observed in persons aged 20-40 years and later in individuals older than 65 years.
Long-term functional outcome after pelvic ring injury has not been well reported. The natural history of unstable pelvic fractures treated nonoperatively has demonstrated a high incidence of residual disability, severe low back pain, and pelvic obliquity and gait disturbances.[19]
Henderson studied 26 patients with nonoperatively treated pelvic fractures at a minimum of 5 years' follow-up.[20] Subjective symptoms included frequent or daily low-back discomfort (50%), localized dysesthesias (46%), and work disability (38%). Objective findings included neurologic deficits (42%), motor weakness or abnormal deep tendon reflexes, and persistent limp (32%). Long-term outcomes correlated well with the amount of residual vertical displacement and the stability of the fracture.
Semba et al also found a correlation between displacement on the initial film and residual symptoms.[21] Patients with a combined anteroposterior and vertical displacement of less than 1 cm at initial injury were asymptomatic, whereas those with a displacement of more than 1 cm at initial injury had an increased frequency of late severe low-back pain.
Gruen et al studied the outcome of patients who had sustained multiple injuries that included unstable pelvic ring injuries and who were treated with ORIF.[22] In this study, 62% of patients returned to full-time work, and most patients with pelvic fractures (77%) had mild disability at 1 year. Persons with open-book injuries tended to have higher individual and total Sickness Impact Profile scores than individuals with LC fracture despite similar Injury Severity Scores.
Tornetta et al reviewed 29 patients with rotationally unstable but vertically stable pelvic ring injuries treated by means of ORIF.[23] The primary indication for surgery was symphyseal disruption. Follow-up evaluation after more than 3 years revealed that 96% had no pain or pain only with strenuous activity. Seventy-six percent ambulated without assistance or limitations, and 76% returned to their preinjury occupation.
Copeland et al found that women with pelvic fractures had higher rates of urinary symptoms, cesarean deliveries, and gynecologic pain (20%) than a matched group of female patients with multitrauma without pelvic fractures.[24] In the pelvic fracture group, 21% had urinary tract symptoms despite a low incidence of frank genitourinary injuries.
Copeland et al postulated that the significant incidence of stress incontinence is due to disruption of the pelvic floor musculature or interruption of its innervations.[24] Urinary tract symptoms were more common in patients with residual pelvic fracture displacement in a lateral or vertical direction as opposed to medial direction. The pelvic floor becomes redundant in individuals with LC injuries, whereas in persons with APC or VS injuries, the pelvic floor is placed under tension and can be disrupted.
McCarthy et al found that in comparison with age- and sex-standardized norms, women with pelvic fractures scored lower on all dimensions of the 36-Item Short Form Health Survey (SF-36), with the exception of mental health.[25]
The outcome of unstable pelvic fractures appears to vary on the basis of the initial displacement, fracture classification, and associated injuries. Long-term outcome studies are required to better determine how operative intervention alters the natural history of these severe injuries.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved