

Tenosynovitis is inflammation of a tendon and its sheath (see the image below). Most acute cases of flexor tenosynovitis (FT)—which involves disruption of normal flexor tendon function in the hand—result from infection. However, FT also can develop secondary to acute or chronic inflammation from a noninfectious cause, such as diabetes, overuse, or arthritis.
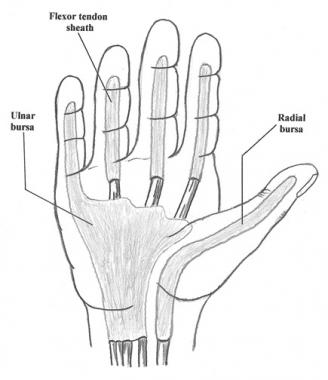 Flexor tendon sheaths and radial and ulnar bursae.
Flexor tendon sheaths and radial and ulnar bursae.
Cases of infectious FT that present early and have no comorbidities have a good prognosis, but patients with fulminant infection, chronic infection, or an impaired immune status have increased risk of long-term complications and impairment.
Infectious tenosynovitis
Patients with infectious FT can present at any time following a penetrating injury, with complaints of pain, redness, and fever. Physical examination reveals Kanavel signs of flexor tendon sheath infection, which are as follows:
Clinical features of gonococcal tenosynovitis include the following:
Inflammatory flexor tenosynovitis
Delayed presentations can have the appearance of fulminant FT with all Kanavel signs or may involve tendon rupture if the patient delays seeking treatment long enough.
See Clinical Presentation for more detail.
If infection is suggested, culture of the suppurative synovial fluid is mandatory prior to beginning definitive antimicrobial treatment. These cultures should include the following samples:
Diagnostic arthrocentesis is indicated if joint effusion is present with tenosynovitis, because most patients with disseminated gonococcal infection have coexistent septic arthritis.
Hematologic studies
Biopsy
Synovial biopsy for histopathologic examination is helpful in diagnosing granulomatous changes observed in Mycobacterium infections and in cases of chronic processes.
Imaging
Obtain standard anteroposterior and lateral radiographs to rule out bony involvement or a foreign body.[1]
See Workup for more detail.
Infectious flexor tenosynovitis
Prompt medical management of acute nonsuppurative flexor tenosynovitis (FT) may preclude the need for surgical intervention. Nonoperative treatment for infectious FT includes the following:
Inflammatory flexor tenosynovitis
Nonoperative management is the primary treatment for inflammatory FT. The mainstay of therapy for FT caused by overuse syndromes is cessation of the insult by modification of activity. Therapy also includes the following:
Treatment for rheumatoid inflammatory FT includes ice, NSAIDs, rest, splinting, hydroxychloroquine, gold, penicillamine, and methotrexate.
Drainage
The indication for surgical drainage includes history and physical examination consistent with acute or chronic FT. In certain circumstances when acute FT presents within the first 24 hours of infection development, medical management may initially be used. Prompt improvement of symptoms and physical findings must follow within the ensuing 12 hours; otherwise, surgical intervention is necessary.
See Treatment and Medication for more detail.
NextTenosynovitis is inflammation of a tendon and its sheath. Most acute cases of flexor tenosynovitis (FT), which involves disruption of normal flexor tendon function in the hand, are the result of infection. However, FT also can develop secondary to acute or chronic inflammation from a noninfectious cause, such as diabetes, overuse, or arthritis. (See Pathophysiology and Etiology.)
Much of the original work on infectious FT was done by Kanavel. Septic FT is diagnosed if a patient presents with the four Kanavel signs, as follows (see Presentation and Workup):
Septic FT has the ability to rapidly destroy a finger's functional capacity and is considered an orthopedic emergency. (See Prognosis, Treatment, and Medication.)
For patient education information, see the Infections Center, as well as Tendinitis and Rheumatoid Arthritis.
Infection can be introduced directly into the tendon sheaths through a skin wound (most often) or via hematogenous spread, as occurs with gonococcal tenosynovitis.
Infectious FT is a closed-space infection. Sheaths of the index, middle, and ring fingers run from the metacarpal neck at the level of the first annular (A1) pulley proximally to the insertion of the flexor digitorum profundus distally. The small finger and thumb sheaths are continuous with the ulnar and radial bursae in the palm, respectively (see the image below). Because the radial and ulnar bursae are contiguous, infections in either the small finger or the thumb are at risk of communicating and potentially progressing to the carpal tunnel.
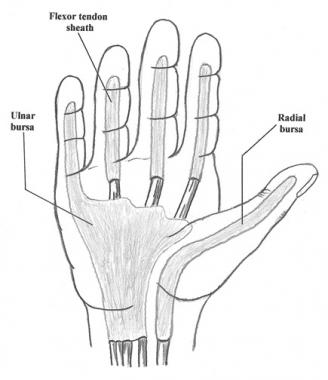 Flexor tendon sheaths and radial and ulnar bursae.
Flexor tendon sheaths and radial and ulnar bursae.
Infection in any of the fingers may spread proximally into the wrist and forearm (Parona space). The initial infection also may move into the fascial spaces within the hand, adjacent osseous structures, or synovial joint spaces, or it may erode through the layers of the skin and exit superficially.
The tendon sheath is made up of an inner visceral layer and an outer parietal layer. Between the two layers is the synovial space, which is filled with synovial fluid. The visceral layer is in close approximation to the flexor tendon. The parietal layer is reinforced by a series of five annular pulleys (A1-5) and three cruciform pulleys (C1-3). The A2 and A4 pulleys are critical for flexor tendon function and should be avoided during surgical manipulation of the infected sheath. (See the image below.)
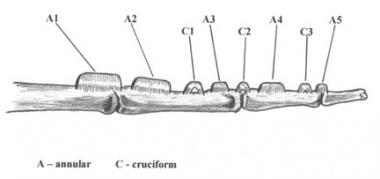 Location of annular and cruciform pulleys on the volar finger.
Location of annular and cruciform pulleys on the volar finger.
With the accumulation of pus in flexor tendon sheath infections, pressure can increase within the closed-space compounds of the flexor tendon sheath, thus inhibiting the inflammatory response. In one study, eight of 14 patients with flexor tendon sheath infections had hand tendon sheath pressure in excess of 30 mg Hg. The increased pressure also inhibits blood flow and adds to the destructive process. Tendon ischemia increases the likelihood of tendon necrosis and rupture.
Flexor tendons of the fingers receive their nutrient supply from a combination of direct vascular sources and diffusion from synovial fluid. An avascular segment of the flexor digitorum superficialis has been found at the proximal phalangeal level. The flexor digitorum superficialis has two distinct vascular supplies, and three have been identified for the flexor digitorum profundus. As a result, the profundus has two avascular segments, which are located over the proximal and middle phalangeal regions.
Inflammatory FT occurs through a process different from the one that produces infectious FT, though it can lead to similar complications. In inflammatory FT, proliferation of fibrous tissue occurs until there is impingement or constriction of the tendon and surrounding structures. The flexor tendons and the flexor retinaculum can create a tourniquet effect, producing distal swelling and pain. Nodularity of the tendons can lead to crepitus and sometimes frank triggering as the tendon becomes impinged adjacent to a thickened segment of the tendon sheath.[2, 3]
Overuse
Overuse syndromes go through predictive stages that can lead to FT. Overuse is defined as repetitive microtrauma that is sufficient to overwhelm the ability of the tissue to adapt. Pathologic stages of overuse include inflammation, proliferation, and, finally, maturation. They proceed as follows:
Several causes of tendon rupture in rheumatoid arthritis (RA) exist. An attrition rupture may occur after the tendon has passed over roughened bony surfaces or has been eroded by chronic synovitis. The tendon also may be weakened by direct invasion of the rheumatoid tenosynovium or by ischemic necrosis secondary to surrounding pressures and diminished vascular supply.
Noninfectious causes of tenosynovitis include the following:
Overuse injury
Overuse syndromes cause cumulative microtrauma to the tendon and tendon sheath. The protective inflammatory process paradoxically leads to tenosynovitis.[8, 9, 2, 3, 10]
In de Quervain tenosynovitis, overuse leads to thickening of the extensor retinaculum of the first dorsal compartment and narrowing of the fibro-osseous canal.
In volar flexor tenosynovitis (ie, trigger finger), overuse is thought to be the most common cause, but multiple etiologies have been identified. The triggering phenomenon is thought to be caused by hypertrophy of the first annular pulley.
Predisposing factors include diabetes mellitus, intravenous (IV) drug abuse, debility, and arteriosclerosis obliterans.
The primary inciting event of infectious FT usually is penetrating trauma, such as a bite wound.[11, 12] Hematogenous spread may occur. Infecting organisms include the following:
Mycobacterium
Several Mycobacterium species have been cultured following animal contacts or simple lacerations/puncture wounds, including the following:
Infection with Mycobacterium species may be suspected in chronic, more indolent infections. Late or missed diagnosis can lead to disastrous outcomes.[15, 16, 17]
Gonococcal infection from Neisseria gonorrhoeae originates as a mucosal infection of the genital tract, rectum, or pharynx. Dissemination occurs in approximately 1-3% of patients with mucosal infection. Approximately two thirds of patients with disseminated gonococcal infection develop tenosynovitis.
Pyogenic FT results from an infectious agent multiplying in the closed space of the flexor tendon sheath and culture-rich synovial fluid medium. Natural immune response mechanisms cause swelling and migration of inflammatory cells and mediators. The septic process and this inflammatory reaction within the tendon sheath quickly interfere with the gliding mechanism, leading to adhesions and scarring. The ultimate consequences are tendon necrosis, disruption of the tendon sheath, and digital contracture.[18, 19]
Infectious flexor tenosynovitis
No data exist regarding the incidence of infectious FT. With penetrating injuries, the possibility of concomitant infection is very high when there is inoculation of the tendon sheath. Infectious FT via hematogenous spread is limited to isolated case reports.
Inflammatory flexor tenosynovitis
The incidence of inflammatory FT is well documented, as follows:
Cases of infectious FT that present early and have no comorbidities have a good prognosis. Patients that present with fulminant infection, those with chronic infection, and those with impaired immune status have increased risk of long-term complications and impairment.
The most common complication in FT is loss of range of motion (ROM) secondary to adhesions. If loss of functional motion persists, tenolysis is considered at 4 months post surgery. One study showed improvement between the 6-week postoperative evaluation and 3-month follow-up.
The second major complication is soft-tissue necrosis, which is more commonly seen in patients with delayed presentation or in those with diabetes.
For patients with inflammatory FT, flexor tendon rupture is a potential complication.
Pang et al conducted a review of 75 patients with pyogenic FT and found that the following risk factors were associated with poorer outcomes[20] :
Eshed et al found that FT that is diagnosed by magnetic resonance imaging (MRI) is a strong predictor of early RA (sensitivity = 60%, specificity = 73%). The investigators also found that an even stronger predictor of RA is the combination of FT on MRI and a positive serum anti-cyclic citrullinated peptide or positive rheumatoid factor.[21]
Another study, by Navalho et al, indicated that MRI offers a better means than Doppler ultrasonography does of predicting the development of RA through the identification of tenosynovitis and carpal joint synovitis. The study involved 45 patients with untreated recent-onset polyarthritis. The hands and wrists of these patients were imaged using 3T MRI and Doppler ultrasonography, and 12 months later the patients were evaluated to determine whether or not their polyarthritis had progressed to fulfill the criteria for RA.[22]
The investigators found that 30 patients met the criteria for RA at follow-up and that 12 months earlier, 3T MRI had identified FT in 86.7% of these patients and also identified carpal joint synovitis in exactly the same percentage of this group. Doppler ultrasonography found FT and carpal joint synovitis in, respectively, 50% and 63.3% of the patients with RA.[22]
Using multivariate logistic regression analysis, the investigators found MRI identification of FT and carpal joint synovitis in early polyarthritis to be a powerful predictive tool in assessing a patient's chance of progressing to RA.[22]
Kameyama et al found evidence that among patients with stenosing FT, those with diabetes have a higher prevalence of multiple joint involvement than do those without diabetes.[23]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved