

The tibial plateau is one of the most critical loadbearing areas in the human body; fractures of the plateau affect knee alignment, stability, and motion. Early detection and appropriate treatment of these fractures are critical for minimizing patient disability and reducing the risk of documented complications, particularly posttraumatic arthritis.[1]
Sir Astley Cooper first described fractures of the proximal tibia in 1825. Anger treated most minimally displaced fractures with early knee traction mobilization.[2] Rausmusen introduced open reduction and internal fixation (ORIF) of tibial condylar fractures, and Sarmiento popularized functional cast bracing of most tibial condylar fractures.[3, 4]
NextThe knee is a complex joint, exposed to forces that can exceed five times the weight of the body. The joint has enhanced mobility at the cost of stability. The proximal tibia expands from the diaphysis through a metaphyseal flare. Contact is made with the head of the fibula in the posterolateral quadrant. The surface of the tibial plateau has a medial and a lateral weightbearing portion and an intercondylar eminence, which is both nonarticular and nonweightbearing. The medial plateau is generally larger than the lateral plateau.
The intercondylar eminence provides attachment to the medial and lateral menisci and the anterior and posterior cruciate ligaments.
The normal knee is in physiologic valgus alignment. Most of the load transmitted across the knee is medial to the eminence, and therefore, the knee has stronger cancellous bone.
Because the medial condyle is rounded as compared with the lateral condyle, some of the anterior articular surface of the lateral plateau is exposed, especially during extension. This causes the lateral plateau to be more susceptible to bone injury and is the reason why fractures of the lateral plateau are more common than those of the medial plateau.
There have been many classifications of tibial plateau fractures,[5] of which the following are probably the most historically significant.
In 1900, Muller proposed a classification system for tibial plateau fractures that categorized fractures according to the amount of articular involvement. Hohl and Luck proposed a classification of plateau fractures that included nondisplaced, local-depression, split-depression, and splitting fractures.[6] Hohl later expanded the classification to include comminuted fractures.[7] In 1981, Moore proposed a classification system for fracture-dislocation of the tibial condyle that took into consideration soft-tissue injury.[8]
Schatzker et al proposed a classification system of condyle fractures based on the fracture pattern and fragment anatomy. This classification system, which is widely accepted and used today, divides these fractures into the following six types[9] :
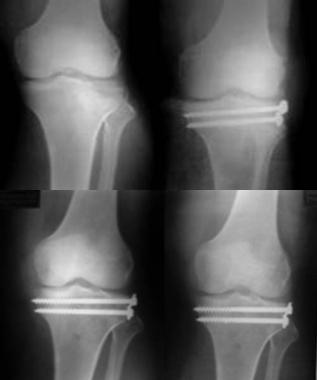 Type II tibial plateau fracture in a young active adult with good bone stock treated with percutaneous elevation and cannulated cancellous screw fixation without bone grafting.
Type II tibial plateau fracture in a young active adult with good bone stock treated with percutaneous elevation and cannulated cancellous screw fixation without bone grafting.
 Type II tibial condyle fracture involving the tibial spine and more than 50% of the medial condyle fixed with biological buttress plating of the lateral plateau.
Type II tibial condyle fracture involving the tibial spine and more than 50% of the medial condyle fixed with biological buttress plating of the lateral plateau.
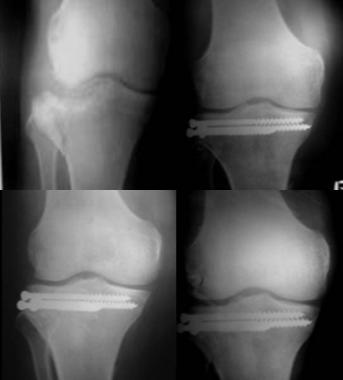 Type III tibial plateau fracture with central depression in an elderly person treated surgically using percutaneous elevation, bone grafting, and cancellous screw fixation.
Type III tibial plateau fracture with central depression in an elderly person treated surgically using percutaneous elevation, bone grafting, and cancellous screw fixation.
 Type IV medial tibial condyle fracture treated with arthroscopy-assisted elevation and percutaneous cancellous screw fixation along with percutaneous screw fixation of the tibial spine fracture.
Type IV medial tibial condyle fracture treated with arthroscopy-assisted elevation and percutaneous cancellous screw fixation along with percutaneous screw fixation of the tibial spine fracture.
 Type VI tibial plateau fracture undergoing biological fixation of the lateral condyle and external fixation of the medial plateau, resulting in an acceptable clinical and radiological result.
Type VI tibial plateau fracture undergoing biological fixation of the lateral condyle and external fixation of the medial plateau, resulting in an acceptable clinical and radiological result.
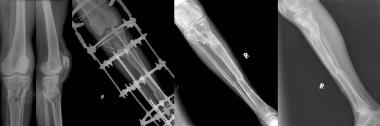 Type VI tibial plateau fracture with severe soft tissue injury successfully treated with Ilizarov external ring fixator.
Type VI tibial plateau fracture with severe soft tissue injury successfully treated with Ilizarov external ring fixator.
 High-energy type VI tibial plateau fracture treated with bone grafting and double plating after the soft tissue condition improved.
High-energy type VI tibial plateau fracture treated with bone grafting and double plating after the soft tissue condition improved.
The most common mechanism resulting in a tibial plateau fracture is a valgus force with axial loading. Of these fractures, 80% are motor vehicle–related injuries, and the remainder are sports-related injuries. A bumper- or fender-related injury from a vehicle-pedestrian collision constitutes more than 25% of tibial plateau fractures. Trauma can be direct or can be related to a fall from a height, an industrial accident, or a sports injury.
Tibial plateau fractures may be either low-energy or high-energy. Low-energy fractures occur in osteoporotic bone and typically are depressed fractures. High-energy fractures occur in low-energy patients often as a result of motor vehicle–related trauma, and the most common pattern of fracture in this group is a splitting fracture.
More than 50% of patients who sustain a tibial plateau fracture are aged 50 years or older. The increased frequency of tibial plateau fractures in older females is due to the increased prevalence of osteoporosis in these individuals. Tibial plateau fractures in younger patients are commonly the result of high-energy injuries.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved