

Hip dislocations, regardless of their etiology, are orthopedic emergencies that require immediate diagnosis, evaluation, and treatment.[1] The adult hip joint is remarkably stable. It is reinforced with thick capsular and labral structures. The presence of a dislocation injury indicates a large force from a traumatic mechanism (a traction force ≥90 lb) or the presence of underlying pathology leading to inherent instability of the joint. Posterior dislocations make up 80-95% of traumatic hip dislocations.
In the presence of a large force injury, Advanced Trauma Life Support (ATLS) measures may need to be initiated in the initial assessment of the patient. Pediatric hip dislocations may occur with smaller amounts of force and have been documented after gymnastic maneuvers and falls from standing. Elderly patients or those with Ehlers-Danlos Syndrome or Down Syndrome are also more likely to dislocate a hip with smaller amounts of traumatic force.
Posterior traumatic hip dislocations occur when the force acts with adduction, internal rotation, and some degree of flexion of the hip. The incidence of this injury has increased as a consequence of high-velocity motor vehicle use.[1] Injuries in which the front-seat passengers are involved in a head-on collision that drives the dashboard into their lower extremities (known as dashboard injuries) have become a notorious cause of posterior traumatic hip displacement. This mechanism of injury is associated with an incidence of simultaneous severe knee injury in 26% of patients, including patellar fractures in 4% of patients.
The increasing popularity of extreme sports has also led to an increase in hip dislocations. One study showed that snowboarders are more likely than skiers to experience hip dislocations.[2] The difficulty in detecting a knee injury in a patient who has a dislocated hip underscores the need for the clinician to maintain a high index of suspicion for multiple lower extremity injuries (eg, acetabular and femoral head, neck, or shaft fractures) as well as occult visceral damage. A review by Onche et al highlighted the high rate of other extremity injuries associated with hip dislocations.[3]
Posterior hip dislocations are also seen following total hip arthroplasty. Relatively minor forces, such as flexing the hip to pick an item up from the floor, can result in post-operative hip dislocation. Several studies[4, 5] indicate that slight alterations in surgical technique (slightly larger femoral head and slightly less acetabular component anteversion) may decrease postoperative dislocation rates.
Multiple studies have demonstrated that the ultimate morbidity for the patient increases as the time interval from injury to reduction increases.[6, 7] Complications such as osteonecrosis of the femoral head, arthritic degeneration of the hip joint, and long-term neurologic sequelae become more likely as reduction is delayed. Whereas the goal is to perform an adequate reduction as quickly as possible, careful prereduction evaluation must be performed to properly diagnose the injury. If adequate closed reduction cannot be attained or if a nerve palsy becomes apparent after closed reduction is achieved, emergency operative reduction is required.
NextClosed reduction is indicated in the following scenarios:
Closed reduction is contraindicated in the following scenarios:
The hip joint (see the image below) is a ball-and-socket synovial joint: the ball is the femoral head, and the socket is the acetabulum. The hip joint is the articulation of the pelvis with the femur, which connects the axial skeleton with the lower extremity. The adult os coxae, or hip bone, is formed by the fusion of the ilium, the ischium, and the pubis, which occurs by the end of the teenage years. The two hip bones form the bony pelvis, along with the sacrum and the coccyx, and are united anteriorly by the pubic symphysis. For more information about the relevant anatomy, see Hip Joint Anatomy.
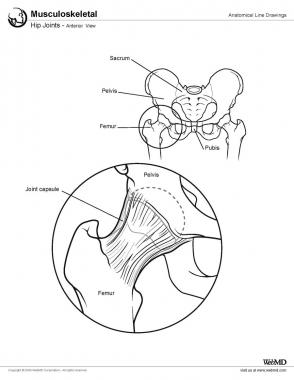 Hip joints, anterior view.
Periprocedural Care
Hip joints, anterior view.
Periprocedural Care
Copyright © www.orthopaedics.win Bone Health All Rights Reserved