

Intertrochanteric fractures are considered one of the three types of hip fractures. The anatomic site of this type of hip fracture is the proximal or upper part of the femur or thigh bone. The proximal femur consists of the femoral head, the femoral neck, and the trochanteric region (including the greater and lesser trochanters). A trochanteric hip fracture occurs between the greater trochanter, where the gluteus medius and the gluteus minimus (hip extensors and abductors) attach, and the lesser trochanter, where the iliopsoas (hip flexor) attaches.
The other two types of hip fractures are fractures of the femoral neck, which are proximal or cephalad to trochanteric fractures, and subtrochanteric fractures, which are distal to or below the trochanters. Although all three types of fractures are commonly referred to simply as hip fractures, the above distinctions between them are important because the anatomy, prognosis, and management are different for each type.
From the early 1800s on, the literature revealed that intertrochanteric hip fractures routinely healed but were malunited in varus, leading to deformity and decreased function secondary to a limp and hip abductor weakness. However, nonoperative care of intertrochanteric fractures had significant, unacceptable morbidity and mortality because of concurrent medical problems and prolonged incumbency that prevented union from occurring. Because of these significant problems, conservative treatment was deemed unacceptable regardless of the mortality.
Therefore, progress in the care of intertrochanteric fractures has involved reducing the mortality from nonorthopedic coexisting or concurrent medical problems and decreasing the degree of malunion and possible nonunion of these fractures. These improvements have allowed patients to become more functional.
The other problem related to intertrochanteric fractures is the associated osteoporosis or osteopenia seen in the aging population. Recognition of this problem has led to the development of programs to ensure that these patients are assessed and, when necessary, treated to prevent a second fracture from occurring. Prevention of the first fracture is also important, in view of the ongoing increase in the elderly population.[1]
Trochanteric fractures are treated by using engineered metallic fixation devices (internal splintage device) designed to maintain the nondisplaced or reduced displaced fracture fragments in an anatomic, near-anatomic, or acceptable position. Fracture stability (the ability of the fracture pattern to resist deformation of weight-bearing) assists in the uncomplicated healing of the fracture. In addition, postoperative care and rates of complications, including mortality and morbidity, vary for the different subcategories of intertrochanteric fractures.
Current treatment of intertrochanteric fractures involves surgical intervention. Despite acceptable healing rates with nonsurgical methods, surgical methods have replaced previous nonsurgical methods of prolonged bed rest, prolonged traction in bed, or prolonged immobilization in a full-body (spica) cast.[2, 3, 4] The acceptable healing rates for nonsurgical management were accompanied by unacceptable morbidity and mortality because of frequent nonorthopedic complications associated with prolonged immobilization or inactivity, as well as malunions compromising patient function.
Such complications included the following:
Currently, with a few exceptions, surgical intervention is used to treat essentially all trochanteric fractures and is described as open reduction and internal fixation (ORIF).
Various internal fixation devices are available to treat essentially all trochanteric fractures. In each case, the appropriate device must be carefully matched to the specific fracture type. The correct surgical technique described by the device developer should also be used. Therefore, the optimal device is chosen after the type of trochanteric fracture has been precisely diagnosed. The indications and contraindications of the technique must also be matched with the patient's activity level, degree of osteoporosis, and realistic expected outcome.
Accomplishing this match between technique and patient requires, at a minimum, technically adequate preoperative radiographs of the hip, including an anteroposterior (AP) view of the pelvis and involved hip and a true lateral view (cross-table technique). In some cases, a frog lateral view, a computed tomography (CT) scan, or even a reconstituted CT scan may be necessary to define the fracture in sufficient detail to permit accurate operative planning. Gentle traction during the radiograph will help define the fracture, particularly if significant shortening has occurred (traction view).
NextThe intertrochanteric area of the femur is distal to the femoral neck and proximal to the femoral shaft; it is the area of the femoral trochanters, the lesser and the greater trochanters (see the image below). The intertrochanteric area can also be seen as the area where the femur changes from an essentially vertical bone to a bone angling at a 45° angle from the near-vertical to the acetabulum or pelvis. The femoral artery and nerve are anterior; the sciatic nerve is posterior. (See Hip Joint Anatomy.)
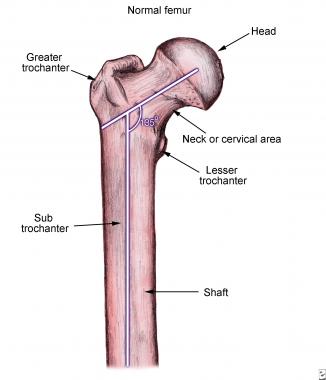 Normal femur anatomy.
Normal femur anatomy.
The attachments of the iliopsoas and the gluteus medius can cause certain displacements, depending on the fracture patterns. These factors may make reduction difficult. The attachment of the gluteus maximus to the lateral femoral shaft is opposite to the posteromedially placed lesser trochanter; it thus acts as a guide to the level of the lesser trochanter and is helpful in the placement of a guide wire for the compression screw. The vastus lateralis overlies the lateral cortex of the proximal femur and must be elevated for application of a side plate.
The stability of an intertrochanteric fracture is defined by the amount of contact between the proximal and distal main fragments (see the images below). A two-part fracture is very stable because once the two fragments are reduced, they are impacted on each other and provide inherent stability for the implant.
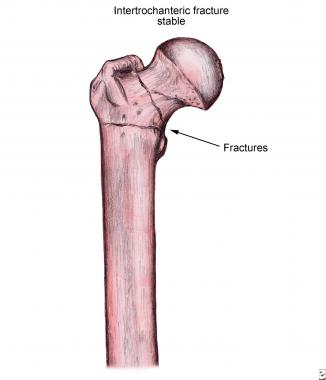 Stable intertrochanteric fracture.
Stable intertrochanteric fracture.
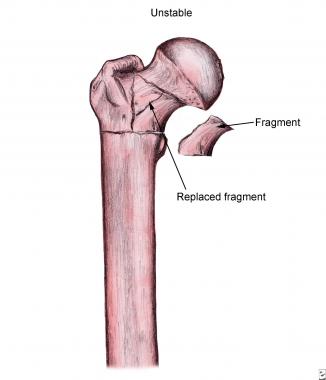 Unstable intertrochanteric fracture.
Unstable intertrochanteric fracture.
In a three-part fracture, the stability of the fracture is inversely proportional to the size of the lesser trochanteric fragment. Instability occurs when more than 50% of the calcar is affected, allowing the proximal fragment to collapse into a varus position and shorten. Therefore, a fracture is considered unstable if there is a large lesser trochanteric fragment or if the greater and the lesser trochanter are separate fracture fragments (four-part fracture).
Another indicator of fracture stability is the intactness of the lateral trochanteric wall,[5] the portion of the greater trochanter that extends form the vastus ridge (the attachment of the vastus lateralis) to the tip of the greater trochanter. If this wall is fractured, the fixation construct will collapse into an unacceptable position, or the implant will cut out.
The more unstable the fracture is, the more difficult reduction will be, and the more likely it is that an implant, such as a cephalomedullary nail, will be needed to stabilize the fracture and prevent collapse.[6] Stable fractures can be treated with a sliding hip screw–plate device (two- to four-hole plate).
Intertrochanteric fractures occur as consequences of either high-energy trauma (rare; seen in young male patients) or simple low-energy falls (common; seen in elderly female patients).
The etiology of low-energy intertrochanteric fracture is a combination of the following factors:
The increasing bone fragility results from osteoporosis and osteomalacia secondary to a lack of adequate ambulation or antigravity activities, as well as decreased hormone levels, increased levels of demineralizing hormones, decreased intake of calcium or vitamin D, and other aging processes.[7] Benign and malignant tumors, along with metastases such as multiple myeloma and other malignancies, can also lead to weakened bony structure.
A direct impact or a torsional force transmitted through the leg to the intertrochanteric area will cause a fracture when such forces are greater than the strength of the bone in the intertrochanteric area.
Approximately 252,000 hip fractures occur each year in the United States. Despite the relatively small incidence, hip fractures are responsible for approximately 3.5 million hospital days in the United States; hip fractures account for more hospital days than tibial fractures, vertebral fractures, and pelvic fractures combined. In addition, hip fractures account for more than half of the total hospital admissions of all fractures and more than half of the ambulance calls for fractures.
Among individuals older than 60 years, intertrochanteric fractures occur more than twice as often in women as they do in men. The mean age for this fracture is 81 years. In this group, the major contributing factors are osteoporosis and the propensity of older patients to fall. In the age group between 11 and 60 years, however, males sustain more fractures than females. The causative factor in this age group is high-energy trauma. It is also more common to see intertrochanteric fractures in Caucasians.[8]
A stable and acceptably fixed intertrochanteric fracture can be expected to heal. In elderly patients, the activity level usually drops by one level after recovery from this injury. The mortality is 20-30% during the first year after fracture for these patients.
A prospective, randomized, single-blind study compared outcomes in patients treated with the Gotfried percutaneous compression plate versus the sliding hip screw for A1 and A2 AO/OTA intertrochanteric proximal femoral fractures.[9] Treatment with the Gotfried plate yielded significantly shorter operating time (48 vs 78 minutes), significantly shorter incision length (56 vs 82 mm), and significantly less blood loss (41 vs 101 mL).
Additionally, the patients treated with the percutaneous compression plate had lower levels of pain with activity, improved quality of life, and a better percent chance of walking independently; however, these latter results were not deemed significant.[9] This study did not differentiate between unstable and stable intertrochanteric fractures (AO/OTA A2.2 and A2.3). As a result, the use of these techniques should be undertaken with caution in unstable fractures.
Unstable intertrochanteric fractures are best treated with an intramedullary device, as indicated by a study of 210 patients randomized to nail versus compression hip screw.[10] Patients treated with such devices had less blood loss, better function and fewer reoperations than those in the compression hip screw group. Similar results were obtained in a randomized, controlled trial of unstable intertrochanteric fractures.[11]
Anglen et al found that from 1999 to 2006, for fixation of trochanteric fractures, there was a dramatic increase in the preference for the use of intramedullary nails that interlock proximally into the femoral head, in comparison with the use of a sliding compression screw.[4] The intramedullary nail fixation rate rose from 3% in 1999 to 67% in 2006. Overall, patients managed with plate fixation had slightly less pain and deformity than those managed with intramedullary nailing, and no significant differences were identified with regard to function or patient satisfaction.
In addition, the authors found that patients managed with intramedullary nailing had more procedure-related complications, particularly femoral shaft fracture.[4] They noted that this change in management of trochanteric hip fractures occurred despite a lack of evidence supporting the change and the apparent potential for increased complications and cost.
Bhandari et al performed a meta-analysis to identify the risk of femoral shaft fracture associated with short cephalomedullary nails after treatment of extracapsular hip fractures.[12] They found that in studies published between 1991 and 2000, gamma nails increased the risk of femoral shaft fracture by 4.5 times when compared with compression screws.
In subsequent studies (2000-2005), however, gamma nails were not associated with significantly increased risk of femoral shaft fracture, and in a 2005 study, there was no difference in femoral fracture rates.[12] According to Bhandari et al, the more recent trials suggest that the increased femoral shaft fracture risk associated with gamma nails has been resolved as the result of improved implant design and better surgical technique.[12]
Sidhu et al studied 53 patients (average age, 77 years) after total hip replacement for trochanteric hip fractures. In the study patients, the Harris hip score at 1 month was 66 ± 7; at 3 months, 72 ± 6; at 1 year, 74 ± 5; at 3 years, 76 ± 6; and at the completion of 5-year follow-up (n = 27), 76 ± 8.[13] The average time to return to normal daily activities was 28 days (range, 24-33 days), and no loosening or infection was observed.
Sidhu et al concluded that in mentally healthy elderly patients with trochanteric hip fractures, total hip arthroplasty may be a valid treatment option because it offers the potential for quick recovery with little risk of mechanical failure, it avoids the risks often associated with internal fixation, and it can enable patients to maintain a good level of function immediately after surgery.[13]
Subsequent studies have shown that the dynamic helical hip system results in outcomes that are comparable to those achieved with the dynamic sliding hip screw, and its blade is more resistant to vertical or rotational displacement.[14, 15]
A meta-analysis of minimally invasive surgery for intertrochanteric fractures reported little difference in the following areas: length of stay, operative time, postoperative pain, complications, mortality, fixation failure, and function.[16]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved