

Cervical spine (C-spine) injuries are the most feared of all spinal injuries because of the potential for significant deleterious sequelae. Correlation is noted between the level of injury and morbidity/mortality (ie, the higher the level of the C-spine injury, the higher the morbidity and mortality). Craniocervical junction injuries are the deadliest.
 Atlantooccipital and atlantoaxial dissociation
Atlantooccipital and atlantoaxial dissociation
 Hangman fracture
Hangman fracture
As many as 10% of unconscious patients who present to the emergency department following a motor vehicle accident (MVA) have C-spine pathology. MVAs and falls are responsible for the bulk of C2 fractures.[1] The clinical manifestations range from asymptomatic to frank paralysis. This article focuses on the uniqueness of and the most common types of traumatic C2 (axis) fractures.
See the list below:
See the list below:
Parker et al retrospectively reviewed the records of 167 patients who underwent posterior cervical fusion with either C2 pedicle (PD) or C2 translaminar (TL) screw fixation and found that breach of PD screws occurred more frequently. In total, 152 TL screws and 161 PD screws were placed. Thirty-one cases of axial cervical fusion (C1-C2 or C1-C3) were performed with TL (16) or PD (15) screw fixation, and 136 cases of subaxial cervical fusion (C2-caudal) were performed with TL (66) or PD (70) fixation. Eleven (7%) PD screws breached the pedicle (0 requiring acute revision), and 2 (1.3%) TL screws breached the C2 lamina (1 requiring acute revision). At 1 year after operation, pseudarthrosis or screw pullout requiring reoperation occurred in 4 (6.1%) patients with TL screws but zero patients with PD screws. The authors noted that 1-year durability of TL screws may be inferior to PD screws for subaxial fusions but equally effective for axial fusions.[2]
Omesis et al found that C2 fractures in the elderly (> 70 y) can be treated surgically with both anterior and posterior approaches with acceptable morbidity and mortality rates and that the majority of patients can be mobilized early and return to their previous levels of independence. Of 29 patients who had undergone surgical treatment for C2 fractures, 25 (86.2%) were able to return to their previous environment.[3]
Chen et al retrospectively compared operative versus nonoperative treatment of closed C2 fractures without spinal cord injury in elderly patients. The primary outcomes of this study were 30-day mortality and complication rates, with length of hospital stay and long-term survival measured as secondary outcomes. The conclusion of this review was that elderly patients faced high morbidity and mortality regardless of the type of treatment, and they should not be excluded from the surgical treatment option based solely on their age.[4]
Nizare et al did a retrospective review of the management of 70 patients with various upper cervical spine injuries. They have concluded that based on good radiological and clinical improvement of the trauma victims, early management of cervical spine injuries could optimize the final outcome.[5]
Stulik et al analyzed the management and prognosis of pediatric patients with unstable upper cervical spine injuries. They found that the majority of these injuries (91.3%) were treated operatively, with the posterior approach used in about two thirds of the patients and with the remaining one third having the anterior approach. The important finding of their study was that despite the relatively frequency of neurological deficits in the pediatric patients with unstable upper cervical injuries, they had a better prognosis than adults, especially for the youngest children with mild deficits. The recommendation from the authors is that therapy for these children should be strictly individualized to maximize positive outcomes.[6]
NextThe unique features of C2 anatomy and its articulations make assessment of its pathology challenging. The odontoid process (dens) is a vertical projection that lies just posterior to the anterior arch of C1, has ligamentous attachments to the skull base, and articulates with C1 (atlas).
The C1/C2 articulation (ie, atlantoaxial articulation) is made up of 3 joints, including the central atlantoaxial joint and the paired lateral atlantoaxial joints. These joints allow rotation of C1 on C2. The transverse ligament of the atlas stabilizes the central atlantoaxial joint, and, together with the odontoid process, acts as a restraint against horizontal displacement of the atlas. The dentate ligament attaches the apex of the odontoid process to the clivus and the paired alar ligaments, which originate from the transverse ligament and attach to the anterolateral rim of the foramen magnum. These ligaments provide rotational and translational stability. The lateral atlantoaxial joints articulate at the superior articular facets of C2 and the inferior articular facets of C1. C2 also is composed of inferior facets, pedicles, transverse processes, and a spinal process.
Incidence of odontoid fractures approaches 15% of all C-spine fractures. Usually, these fractures are secondary to MVAs or falls.[3] When an odontoid fracture is suspected, it is important to rule out concomitant associated C-spine injuries. For example, C1 anterior ring fractures are not an uncommon finding, and a prevertebral soft-tissue shadow of more than 10 mm on plain films is highly suggestive of such a fracture. Anderson and D'Alonzo classified odontoid fractures based on the anatomic location of the fracture (see the image below).
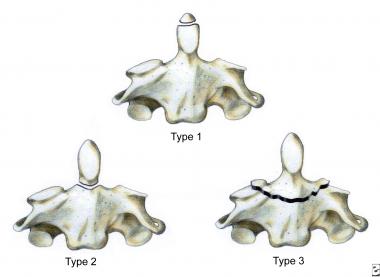 Three types of C2 odontoid fractures: type I is an oblique fracture through the upper part of the odontoid process; type II is a fracture occurring at the base of the odontoid as it attaches to the body of C2; type III occurs when the fracture line extends through the body of the axis.
Three types of C2 odontoid fractures: type I is an oblique fracture through the upper part of the odontoid process; type II is a fracture occurring at the base of the odontoid as it attaches to the body of C2; type III occurs when the fracture line extends through the body of the axis.
See the list below:
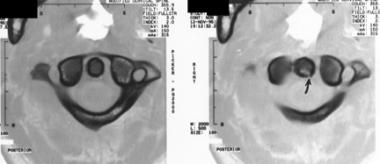 Odontoid type II fracture
Odontoid type II fracture
The precise mechanism of odontoid fractures is unknown. However, the mechanism most likely includes a combination of flexion, extension, and rotation. In addition to pain and inability to actively move the neck, most patients complain of a sensation of instability, described as a feeling of the head being unstable on the spine. Patients may present by holding their head with their hands to prevent any motion. Clinical findings range from quadriplegia with respiratory center involvement to minimal upper extremity motor and sensory deficits secondary to loss of 1 or more cervical nerve roots. Radiographic findings are based on the type of fracture.
An isolated C2 lateral mass fracture is extremely rare and usually is found serendipitously when evaluating for other C2 traumatic pathology. If a C2 lateral mass fracture is found, other C-spine pathology must be sought. The mechanism of this fracture is axial compression with concomitant lateral bending.
Signs and symptoms of concomitant C-spine pathology tend to dominate the clinical picture. The isolated fracture may present with high neck pain and a normal neurological examination. Radiographic findings include impaction of the C2 component of the atlantoaxial articulation surface, asymmetry of C2 lateral mass height, and lateral tilting of the arch of C1. Atlantooccipital and atlantoaxial dissociation can be seen in the image below.
 Atlantooccipital and atlantoaxial dissociation
Atlantooccipital and atlantoaxial dissociation
C2 extension teardrop fractures are avulsion fractures with an intact anterior longitudinal ligament displacing and anteriorly rotating the anteroinferior vertebral body fragment. The avulsed fragment's vertical dimension equals or exceeds its transverse dimension, and focal and minimal prevertebral soft-tissue swelling usually is present. This type of fracture tends to occur in elderly patients with osteoporotic bone. As the name implies, this type of fracture is the result of extension forces.
C2 extension teardrop fractures tend to be stable, and usually are not directly responsible for spinal cord injury. These fractures are extremely rare and differ in many aspects from flexion teardrop fractures that are more common of the lower C-spine. Although lower C-spine teardrop fractures can result from extension forces, they usually result from severe flexion forces. These fractures are unstable and are associated with anterior cord syndrome (quadriplegia; loss of pain, touch, and temperature sensations, but with retention of posterior column functions – proprioception and vibration), secondary to impingement of the cord by the hyperkyphotic vertebral segment or, more commonly, by retropulsion of C2 into the canal. C2 extension teardrop fractures are associated with traumatic spondylolisthesis of C2.
A great deal of confusion surrounds the exact pathology of this fracture. The modern origin of this confusion seems to be in a paper published by Schneider in 1964, wherein the term "hangman's fracture" was given to fractures sustained in MVAs that had radiographic similarities to fractures resulting from judicial hangings. In 1964, Garber suggested the term traumatic spondylolisthesis for the more common injury pattern usually seen as a result of falls and MVAs. The injury pattern seen secondary to judicial hangings is a fracture-dislocation of C2. More precisely, it is a bilateral pedicle fracture of C2, along with distraction of C2 from C3 secondary to complete disruption of the disk and ligaments between C2 and C3. The injury pattern seen secondary to MVAs and falls also is a bilateral pedicle fracture, but differs from the judicial hanging injury pattern with respect to varying degrees of disk and ligamentous disruption and secondary C2/C3 distraction.
The mechanism of a hangman fracture (see the image below) is a combination of hyperextension and distraction. The mechanism of the traumatic spondylolisthesis fracture pattern primarily is hyperextension with varying degrees of axial compression and lateral flexion. Without the primary distraction force, there are varying degrees of disk and ligamentous disruption and secondary C2 displacement.
 Hangman fracture
Hangman fracture
Traumatic spondylolisthesis is a common C-spine injury in fatal MVAs, and only occipitoatlantal dissociations occur more often. Up to one third of patients sustaining this injury have additional C-spine pathology, and up to 10% of patients have noncervical spinal pathology. Craniofacial and vertebral artery injuries are not uncommon findings. Interestingly, neurologic sequelae from spinal pathology are not as common as might be expected. This is due to the autodecompression of the spinal canal that takes place secondary to bilateral pedicle fractures.
Levine and Edwards recently modified a classification system that was proposed by Effendi. This classification system categorizes C2 fractures based on the degree of displacement on lateral C-spine radiographs and on mechanical stability. This system is useful in reconstruction of the injury mechanism and in mapping out a treatment.
The workup of suspected C2 fractures relies on imaging. Plain film, CT scan, and MRI are all employed.[7, 8] Plain film views should include anteroposterior (AP), lateral, and odontoid views..[9, 10] Additionally, some authors recommend oblique views to better assess the posterior elements. (For specific radiographic findings, see the section Common C2 Fractures.)
Plain films tend to be better than CT for detecting subluxations and dislocations; CT usually is better for detecting most fractures and for characterizing the extent of the pathology. Most of the fractures missed on CT are those oriented in the axial plane or those involving the odontoid process. Plain film also is better for detecting vertebral body and spinous process fractures. Plain films are used routinely as the study of first choice; if pathology is found, CT usually is performed next to help define the extent of the injury. If the plain film studies are not diagnostic and clinical suspicion remains high, then further evaluation using CT is mandatory.
Some clinicians advocate the use of 3D CT reconstruction as both a diagnostic aid and a surgical template. However, its role has yet to be characterized fully. The role of MRI in spinal trauma is to aid in the characterization of soft-tissue injury, neural element injury, and disk injury. This is the study of choice for the evaluation of ligamentous and spinal cord injury, and is mandatory in any trauma patient with a neurologic deficit.
Treatment for type I fractures is hard-collar immobilization for 6-8 weeks, which usually is quite successful.
Type II fractures can be managed conservatively or surgically. Treatment options include the following:
Arthrodesis can be accomplished by C1/C2 transarticular screw fixation, interlaminar clamps, or wiring techniques such as the Gallie or the Brooks method.[12, 13, 2, 14]
Management with the halo vest usually is considered if the initial dens displacement is less than 5 mm, the reduction is performed within 1 week of the injury and is able to be maintained, and the patient is younger than 60 years. During immobilization, alignment is assessed to ensure that reduction is maintained. Displacement of less than 20% is acceptable. The halo vest is in place for 12-16 weeks and the fusion rate is over 90%.[15]
Wiring techniques, such as Gallie or Brooks methods, offer a high fusion rate (about 95%); however, the posterior arch needs to be intact and a halo vest must be worn postoperatively. Transarticular screw fixation provides a high fusion rate and the posterior arch need not be intact. Although posterior surgical fusion techniques provide high fusion success rates, they do so at the expense of cervical rotation. Generally, up to 50% of rotation is lost with these techniques.
Nonunion, malunion, and pseudarthrosis formation are potential major complications. Factors affecting this are amount and position of displacement, degree of angulation, ability to obtain and hold a reduced fracture, age of the patient, and tolerance to halo immobilization. However, some reports have demonstrated nonunion rates approaching 80% in certain subsets of patients. Shilpakar et al looked at all treatment options and associated rates of complications.[16] On the basis of a meta-analysis of previously published studies, they concluded that type II fractures are best managed with odontoid screw fixation.
Anterior odontoid single screw fixation is noted to preserve normal rotation at C1/C2, provide immediate stability, and obviate the need for postoperative halo immobilization. Furthermore, rates of malunion, nonunion, and pseudarthrosis formation are very low. There are limitations to this approach, namely, the age of the fracture and the patient's body habitus. If the fracture is more than 4 weeks old or if the patient possesses a short neck and barrel-shaped chest, consider an alternative treatment approach, such as transarticular screw fixation or Brooks sublaminar fusion.
There has been some controversy regarding operative versus nonoperative management of type II fractures. Vaccaro et al, in a study of 159 elderly patients with type II dens fractures, reported a significant benefit with surgical treatment and recommended that elderly patients with such fractures who are healthy enough for general anesthesia be considered for surgical stabilization.[17]
The investigators from the AOSpine North America Geriatric Odontoid Fracture Mortality Study did not find operative treatment of type II fractures to have a negative impact on survival in 322 elderly patients with type II fractures, even after age, sex, and comorbidities had been adjusted for.[18] In this study, operative treatment had a significant advantage in 30-day survival advantage, and a trend toward improved longer-term survival was noted.
Paolo et al examined 108 consecutive type II fractures, of which 60 were conservatively treated with external immobilization and 48 surgically treated .[19] They concluded that all odontoid fractures without dislocation should be treated with rigid external immobilization and that all odontoid fractures with dens dislocation exceeding 5 mm should be considered for surgery. They further suggested that type II fractures in patients older than 50 years should also be considered for surgery; outcomes with conservative treatment are better for patients younger than 50 years.
Type III fractures are treated with halo immobilization, odontoid screw fixation, or C1/C2 arthrodesis. Deep, displaced, or angulated fractures are treated with closed reduction and halo thoracic immobilization. Uncomplicated shallow type III fractures are treated with odontoid screw fixation. Nonunion and malunion are potential complications. The vertical type of odontoid process fractures is addressed in the treatment section on traumatic spondylolisthesis.
A prospective, controlled study evaluated the safety and efficacy of percutaneous anterior screw fixation for type II and rostral type III odontoid fractures. Using clinical and radiographic results from 42 patients who underwent percutaneous anterior screw fixation or open screw fixation, the data found significantly less operating time and less blood loss in the percutaneous anterior screw fixation group. Both groups experienced satisfactory bony union, similar radiation time, and clinical outcome, and no evidence of abnormal movement at the fracture site was noted. These data suggest that percutaneous anterior screw fixation may be a safe and reliable alternative with potential advantages for treatment of type II and rostral type III odontoid fractures.[20]
Another study evaluated the outcomes after anterior screw fixation of type II and rostral shallow type III fractures. The study found that the risk of fusion failure was 37.5 times greater in patients in whom surgery was delayed for more than 1 week and 21 times greater in patients with a fracture gap of greater than 2 mm.[21]
Treatment ranges from collar immobilization for uncomplicated minimally depressed fractures to cervical traction followed by halo immobilization for more extensive fractures. Complications secondary to posttraumatic degenerative changes may eventually warrant atlantoaxial arthrodesis.
Treatment of these fractures is cervical orthosis, unless more aggressive measures are needed to secure a concomitant unstable fracture.
Treatment of type I fractures usually is with a Philadelphia collar or halo. Several treatment options are available for type II fractures, the first being conservative external fixation with halo or tong traction in weighted extension for 1 week. If reduction is acceptable (with less than 4 mm of displacement and less than 10 degrees of angulation), treatment progresses with halo-vest immobilization for 12-16 weeks. If reduction is unacceptable, weighted extension traction resumes for up to 6 weeks, followed by halo treatment for 6 weeks. If adequate results are not achieved after closed reduction and traction, open reduction with anterior cervical plating is the next step. The other surgical treatment option consists of weighted extension traction to accomplish adequate reduction, followed by internal fixation with a C2 transpedicular screw. Conservative and surgical treatments typically yield excellent results.[11, 15]
Treatment options for type IIA fractures include both conservative and surgical measures. Conservative treatment consists of closed reduction that is obtained under fluoroscopic guidance via application of compression and extension and is followed by halo-vest immobilization. Repeated imaging is used to monitor the healing process with a variable time course. Surgical options include C2 transpedicular screws and anterior cervical plating. Conservative and surgical treatments typically yield very good results. Malunion is a potential complication.
For type III fractures, surgery is indicated if the fracture line extends anteriorly to the facet dislocation, at the level of the dislocation, or just posterior to it. Any of these locations make reduction unlikely secondary to instability. In this case, surgical reduction and stabilization is mandated and is accomplished with lateral mass plates, interspinous wiring, or bilateral oblique wiring. Once accomplished, bilateral pedicle fractures can be addressed with C2 transpedicular screws, or treated conservatively with traction or a halo/vest. Lateral mass plating of C2 by placing lateral mass screws in C3 in conjunction with C2 transpedicular screws may make postoperative halo immobilization unnecessary.
Atypical traumatic spondylolisthesis fractures are managed on a case-by-case basis, weighing the need for more aggressive stabilization against the likelihood of fragment dislodgment and subsequent spinal cord injury. Surgical treatment options for these fractures include C2 transpedicular screw fixation along with odontoid screw fixation.
For all types of traumatic spondylolisthesis fractures, nonunion and malunion are the major complications of nonoperative treatment, but, fortunately, these are rare occurrences.
Complications of C2 fracture treatment are nonunion, malunion, pseudoarthrosis formation, infection, neurovascular injury, acute airway compromise, and hardware failure. The risks of nonunion, malunion, and pseudoarthrosis formation are lessened with surgical treatment.[22] As with any surgical procedure, risk of infection always exists. Osteomyelitis is a rare, but not unknown, complication. Some authors recommend the use of prophylactic antibiotics for up to 72 hours following surgery, and continuation if there is evidence of an infection. Neurovascular injury is a risk associated with any surgical intervention and is a function of both surgical acumen and anatomic variability. Airway compromise is a risk associated with any anterior surgical approach, and prolonged endotracheal intubation may be necessary. Common hardware failures include screw bending and breaking, loosening of implants, and hardware failure secondary to osteoporotic bone.
Follow-up is critical for any patient sustaining a C2 fracture. In addition to the clinical examination, repeat imaging studies are warranted. Generally, the various treatment modalities used for C2 fractures are quite successful. The only outcome data currently available are for surgical treatment of type II odontoid fractures. A meta-analysis showed that single screw odontoid fixation using the anterior approach yielded better results than those found with transarticular fusion, multiple screws, or closed reduction with halo vest immobilization.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved