

Fractures of the tibia and the fibula are the subject of ongoing controversy and discussion. Despite newer innovations in implants and external fixation devices, tibial fractures essentially remain unresolved; they are among the most challenging fractures to be treated by an orthopedic surgeon. These injuries are different and variable in presentation, and their outcomes are unpredictable.
The literature has traditionally included two schools of thought regarding management of these injuries: operative and nonoperative therapy. Although gray zones have been resolved, no consensus has been reached on the optimal management of diaphyseal fractures of the tibia. This problem is predominantly attributed to the high prevalence of concomitant closed and open soft-tissue injuries. Therefore, diaphyseal tibial injuries are prone not only to infection and nonunion in the long term but also to significantly increased morbidity caused by polytrauma and associated injuries in the acute setting.
The delayed unions and nonunions that occur in these fractures are themselves a separate problem covered extensively in the literature and in academic forums. As Marvin Tile wrote:[1]
"We should reject the theories of the dogmatists who say that all tibial fractures should be treated operatively or that all tibial fractures should be treated nonoperatively. It is time to remove this kind of dogma from one's thinking and to individualize the treatment of these fractures. The optimal treatment of a tibia fracture stems from an analysis of the natural history of the fracture. A thorough assessment of the fracture type and pattern and then correlating it with the natural history of a similar fracture type permits achievement of the best functional outcomes for each individual patient."[1]
The ability to treat tibial shaft fracture by conservative or operative means depends on what is often termed the natural history of the fracture. John Charnley hypothesized that the periosteal hinge was the important factor in the management of fractures. Conservative management was more likely to fail in fractures that had a residual fracture gap or an intact fibula than in others. Some factors that influence the natural history of tibial fractures include the location and extent of displacement, comminution, soft-tissue injury, and contamination. Another factor is antecedent sepsis.
The Edwin Smith papyrus (an ancient Egyptian treatise on trauma surgery from the 17th century BCE) contained references to the management of long-bone fractures with splints and bandages. Hippocrates recommended the use of bandages and splints in his treatise on fractures; he stressed the need to change these bandages frequently to accommodate changes in limb swelling.
The advent of plaster and the design of functional casts revolutionized the management of tibial fractures.[1, 2, 3, 4] Anthonius Mathijsen, Fedor Victor Krause, Pierre Delbet, and, more recently, Augusto Sarmiento have considerably refined the indications and methods of conservative management of tibial fractures. Understanding wound debridement and knowing Sir Joseph Lister's work on antisepsis enabled surgeons to treat open diaphyseal tibial fractures with some prospect of avoiding amputation.
Albin Lambotte first pioneered external fixation in the tibia, and Ernest William Hey Groves introduced internal fixation with nails, which Gerhard Küntscher and J Otto Lottes later popularized. The AO (Arbeitsgemeinschaft für Osteosynthesefragen) school further refined the practice of intramedullary nailing and interlocked nailing.
NextKnowledge of the relevant anatomy is essential for recognizing and planning management of the soft-tissue injuries that are associated with diaphyseal tibial fractures.
The tibia is triangular in cross-section, with proximal and distal flares. It has three surfaces: medial, lateral, and posterior. This bone is thinnest in cross-section at the junction of the middle and lower thirds. The anteromedial border is subcutaneous throughout its length and is called the shin. The broad and smooth medial surface is also subcutaneous throughout its length.
The nutrient artery to the tibia arises from the posterior tibial artery, which enters the tibia at the posterolateral cortex distal to the origin of the soleus at the oblique line of the tibia. Inside the medullary canal, it gives off three ascending branches and one descending branch, which form the endosteal vascular tree. This, in turn, anastomoses with the periosteal vessels originating from the anterior tibial artery.
As it passes through a hiatus in the interosseous membrane, the anterior tibial artery is particularly prone to injury in diaphyseal fractures of the tibia. The peroneal artery has an anterior communicating branch to the anterior tibial artery. Hence, an occlusion of the peroneal artery may exist, even in the presence of a dorsalis pedis pulse. The distal third of the tibial shaft is supplied by the periosteal anastomoses around the ankle, with branches entering the tibia through ligamentous attachments. A watershed zone may exist at the junction of the middle and lower thirds of the tibial shaft.
When the nutrient artery is obstructed, reverse flow is established through the cortex. In such a situation, the periosteal blood supply becomes more important. This situation emphasizes the importance of preserving the periosteal attachments during fixation procedures.
Tight osteofascial compartments surround the tibia. The crural fascia divides the leg into four compartments; one of these is for the weaker muscle group of extensors, and the other three serve the stronger flexor musculature.
The compartments of the leg are as follows:
The septa are as follows:
The pathoanatomy of the fracture includes the location, morphology, and soft-tissue status of the limb. Because of its subcutaneous location, the tibia is extremely prone to soft-tissue injury and compounding (see the image below). This damage can occur at the time of injury or at the time of surgery. Closed soft-tissue trauma can be significant and may go unrecognized.
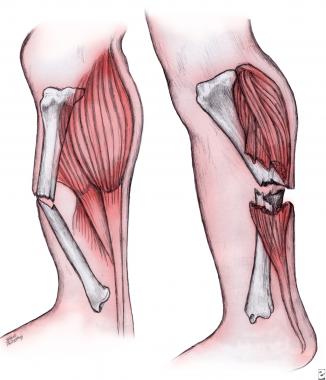 Mechanism of compounding.
Mechanism of compounding.
Diaphyseal fractures are slow to heal and are often unpredictable in terms of their course to union. Trauma is greater with long, spiral fractures than with transverse and short oblique fractures. The degree of trauma is further manifested in the extent of the comminution and displacement, both of which are also indicative of extensive soft-tissue disruption. Soft-tissue damage may be overt or may be a frank open injury.
Ipsilateral limb fractures, polytrauma, visceral injuries, and comorbid factors, such as the patient's general condition and age, as well as coexistent arterial or nerve injuries, also markedly influence outcomes.
Good nonoperative management is preferred to bad operative management.
The mechanism of a diaphyseal tibial injury can be direct or indirect. Direct mechanisms of injury are high-energy fractures (road traffic accidents), penetrating injuries, and three-point bending injuries. High-energy mechanisms produce transverse or comminuted displaced diaphyseal injuries, with a higher incidence of compounding and soft-tissue injury.[5, 6]
Penetrating injuries (eg, gunshot wounds) may produce a variable pattern, depending on the missile involved in the injury. Bending forces (eg, ski-boot injuries) produce short, oblique, spiral fractures and sometimes a small butterfly fragment. On occasion, a highly comminuted segmental pattern of injury may be observed. The prevalence of open and closed soft-tissue injuries is high.
Indirect mechanisms are primarily torsional, low-energy injuries, which produce spiral, nondisplaced, minimally comminuted fractures with minimal soft-tissue damage.
Tibial fractures are among the most common lower limb injuries to be treated by an orthopedic surgeon. In the early 1990s, tibial fractures accounted for 77,000 hospitalizations per year. The incidence has increased to approximately 500,000 cases in the United States per year. On average, almost 26 tibia fractures occur per 100,000 population per year.
An epidemiologic analysis of open long-bone fractures at the Edinburgh Orthopaedic Trauma unit was performed over 6 years.[4] The authors also analyzed 2450 consecutive fractures of the tibia and the fibula over 3 years.[7] Of these fractures, 21.3% were diaphyseal.
The average age of affected patients rises almost linearly as the injuries progress from AO type A to AO type C (see Workup, Staging). The most common causes are road traffic accidents and sporting injuries. Open fractures account for 23.5% of these fractures, with Gustilo grade 3 being the most frequent of the 3 types. Only 8% were grade 3C, requiring vascular reconstruction.
Results of a later study of open fractures showed that the severity of injury represented by the fracture index was correlated with the injury severity score for each fracture type and location.[8]
Approximately 21% of patients who present with open fractures have considerable musculoskeletal injuries. Those with open femoral fractures tend to be most severely injured. Patients with distal tibial fractures tend to have an injury severity score and a fracture index that are lower than those of patients with diaphyseal tibial fractures. Most vascular injuries occur in persons with diaphyseal fractures, and most of these persons eventually undergo amputation.
The average age of those with a tibial fracture is approximately 37 years, with an average of 31 years for men and 54 years for women. Data indicate a bimodal distribution, with a preponderance in young men. In fact, the highest incidence of adult diaphyseal tibial fractures is seen in male adolescents aged 15-19 years, in whom the incidence is approximately 109 cases per 100,000. The second peak, which appears after age 80 years, especially affects the female population and is attributed to osteoporosis. However, a change in demographic patterns can be expected with the institution of stringent gun control laws and better road safety measures.
The outcome and prognosis of a diaphyseal tibial fracture depend on what Brumback and Virkus and Tile called the "personality" of the fracture. Other factors include the location of the fracture, the extent of comminution (which signifies the extent or energy of the trauma), the degree of soft-tissue trauma, the presence of comorbid factors (eg, diabetes), and the presence of polytrauma. Limb-threatening vascular and nerve injuries also substantially alter the patient's prognosis.
The outcomes vary and are universally worse with higher grades of compounding and closed soft-tissue injuries. The method of treatment is also a contributory factor.
In the acute setting, distal vascular injuries are associated with an increased rate of amputation and poorer results after limb salvage. Higher rates of nonunion, delayed union, infection, and amputation are seen in patients with higher grades of soft-tissue and bony injury.
Predictors of secondary procedures in a tibial fracture are an open fracture, a transverse fracture, and a postoperative fracture gap. Smoking and comorbid factors also increase the rate of nonunions. Delayed union is reported in as many as 16-60% of low-energy injuries and 43-100% of Gustilo type 3B injuries.
When the use of external fixators is the primary management, the rate of infection increases with conversion to intramedullary nails, irrespective of the care taken before nailing, with respect to pin-track healing. The prevalence of delayed union and nonunion is also high in fractures with extensive comminution or instability that are treated using nonoperative methods.
The rate of infection and soft-tissue breakdown is sufficiently high with conventional plate techniques that they might be better avoided altogether. However, early results with minimally invasive plate osteosynthesis and locked compression plates are encouraging; the procedures are indicated in selected patients with articular extension and metaphyseal comminution.
Long periods in a functional brace or cast uniformly gives rise to severe hindfoot disabilities. Notably, however, these methods have yielded the best results in patients with low-energy fractures.
Intramedullary nailing is the benchmark in the treatment of diaphyseal long-bone fractures. The results are consistent and predictable, and the complications are easily manageable. Infection rates have been low in most series, with rates of infection being higher in Gustilo grade 3 injuries than in others. In these cases, using an unreamed nail may be judicious. All other fractures, including grade 1, grade 2, and low-grade closed fractures with soft-tissue injury, can be treated with reamed nails. Unreamed nails are best in Gustilo grade 3B injuries. Note, however, that the use of unreamed nails is associated with a significant risk of implant failure.
A Cochrane review on intramedullary nailing of the tibia failed to find significant conclusive evidence in favor of either reamed or undreamed nailing. However, reamed nailing appeared to have a lower risk of nonunion and implant failure compared with unreamed nails.[9]
The degree of reaming does not have any statistically significant influence on the outcomes of nailing; however, more aggressively reamed tibias tend to have faster healing times and faster return to function.[10]
A French study of 28 cases of isolated tibial fractures found intramedullary nailing to be a useful mode of treatment to prevent nonunion and varus angulation in tibial fractures without fibular fractures. Intramedullary nailing is the preferred first-intention mode of treatment in these injuries.[11]
A review of a about 323 cases of open tibial fractures treated in Singapore showed that there was no difference in infection rates even if the fractures were operated on within 6 hours of admission. The authors found complication rates to be much higher amongst multiply injured patients.[12]
With the increase in incidence of high-velocity road traffic accidents, there has been an increase in the incidence of open fractures of the tibia. Debridement is the mainstay of treatment to manage the soft tissue injuries. However, stabilization of the bone is as important as the soft-tissue management to ensure healing of the osteocutaneous injuries. These injuries are also associated with greater incidence of vascular and nerve injuries, which may affect the postoperative course and functional prognosis following injury.
Traditionally, these fractures were treated with wound debridement and external fixation followed by soft-tissue coverage and bone reconstruction. The period of treatment would last from months to years. There is an increasing trend to offer single-stage management of these injuries with internal fixation and early flap coverage to improve functional results.
Gopal et al described the acute management of these fractures with the dictum of "fix and flap" using immediate intramedullary nailing and early or immediate soft tissue coverage, with encouraging results.[13] They suggested immediate or early referral to a suitable center equipped with plastic- and super-speciality services as early as possible.
In another paper analyzing the outcomes of open tibial fractures over 9 years in Singapore, it was observed that the more severe injuries of the tibia were often associated with polytrauma, increased hospital stays, and multiple reoperations. The severity of polytrauma may determine feasibility of early surgery within 6 hours; the authors mention no significant benefits of surgery within 6 hours in this subset of patients.[12]
The special issues incurred in addressing open tibial fractures sustained in combat were assessed and described in a paper by Penn-Barwell et al.[14] The authors noted the need for aggressive prevention of infection and the need for orthopedic plastic surgical management. They also noted the tendency for poorer bony healing in this group of patients. They had an amputation rate of 13%. They did not find a relationship between the mode of fixation and the final functional outcomes.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved