

One of the most challenging roles of the team physician involves the intervention and decision-making processes regarding cervical spine (C-spine) injuries in contact sports. The team physician must be well versed in the prevention, evaluation, stabilization, and treatment of C-spine injuries.[1] A high index of suspicion and an understanding of cervical alignment and architecture, as well as comprehension of the mechanics exerted during a sporting event, are imperative to diagnosing cervical injuries.[2, 3]
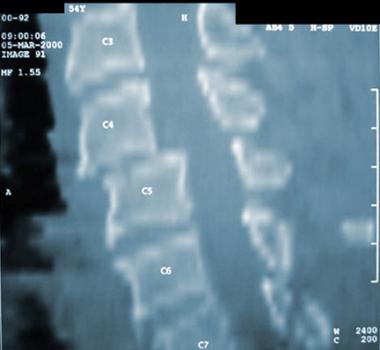
The image below depicts a three-dimensional CT scan of C1.
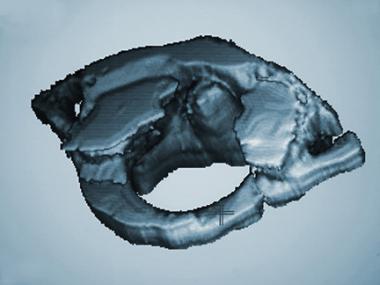 Three-dimensional CT scan of C1.
Three-dimensional CT scan of C1.
See Football Injuries: Slideshow, a Critical Images slideshow, to help diagnose and treat injuries from a football game that can result in minor to severe complications.
Well more than half of catastrophic injuries in sports are cervical spine injuries. C-spine injuries have been reported in most contact sports, including football, hockey, rugby, and wrestling, as well as in several noncontact sports, such as skiing, track and field, diving, surfing, power lifting, and equestrian events. C-spine injuries are estimated to occur in 10-15% of all football players, most commonly in linemen and defensive players. Serious injuries with neurologic sequelae remain infrequent, and most of these injuries are self-limited. Injuries occur in all levels of play, from the high school to the professional level.[4, 5, 6, 7, 8]
Football and rugby have the highest incidence of C-spine injuries of all sports.[9, 10, 11] Injury usually is secondary to high-velocity collisions between players, causing acceleration or deceleration of the head on the neck.[12] Acceleration usually causes a whiplash type of extension force on the neck, while deceleration usually results in flexion forces.[13] Spearing, which has been banned in American football since 1976, occurs when a player uses the helmet/head as the first point of contact with another player. Spearing is a significant cause of C-spine injuries and quadriplegia. The force transmitted to the cervical spine in these cases is one of axial compression with the vertebrae in positions of slight flexion.[14]
The natural architecture of the normal C-spine assumes a lordosis of the vertebrae. This lordosis allows for controlled motion and the transmission of forces to the supporting muscles and soft tissues. When the neck is slightly flexed, approximately 30°, the normal lordosis is straightened, and the forces of the axial load are transmitted to the bones and disks. If the impact force is greater than the yield strength of the vertebrae, a fracture and possible dislocation with cord injury can occur.[15, 16]
Cervical injuries that result from participation in sports usually are self-limited and can be divided into the following categories:
The optimal imaging strategy for the spine is often unclear. Conventional imaging has long been the primary imaging modality of choice for the cervical spine, but there is now evidence to suggest that multidetector computed tomography (CT) may be preferable for cervical spine injury.[17] However, this may not be the case for children and adolescents.
Hannon et al conducted a study to determine the optimal means of evaluating pediatric patients with cervical spine injury from blunt trauma. In patients requiring imaging, screening radiography was the preferred modality in conjunction with focused CT.[18] CT was preferred when the probability of cervical spine injury was 24.9% or higher. The investigators concluded that in a hypothetical pediatric trauma population, clearing and screening radiographs are preferred for evaluation and that CT is rarely optimal for initial evaluation.
Next{refNerveRootBrachialPlexusInjuries}[[19] 19] The most common cervical injury in football players is the transient loss of function with searing or lancing pain down one arm following a collision. These are colloquially referred to as stingers, or burners.[20, 21] Prospective studies performed at Tulane University have shown a 7.7% incidence of stingers in a group of college football players. Initially, the player complains of total arm weakness and a radiating burning sensation that usually resolves. Numbness in the C-6 dermatomal distribution may persist. Motor weakness of shoulder abductors, elbow flexors, external humeral rotators, and wrist and finger extensors also may persist. The duration of symptoms is from 2-10 minutes to 24 hours. Symptoms are reproduced by the Spurling maneuver. Function gradually returns from the proximal muscle groups to the distal muscle groups.
The severity of the injury correlates with the underlying pathophysiology. Neuropraxia is a selective demyelination of the nerve sheath, and it is the most benign injury. Axonotmesis is a disruption of the axon and the myelin sheath, but the epineurium is intact. The most severe injury is a neurotmesis or a compete disruption of the endoneurium. This injury is associated with the most unfavorable prognosis.
The differential diagnoses of burners include acute cervical disk herniations, foraminal stenosis, and extradural intraspinal masses.
Stingers are thought to be the result of either of the following mechanisms:
Because most burners are self-limited, the most important treatment obligation of the team physician is to rule out an unstable cervical injury. The key to assessment is that patients with burners have full pain-free neck range of motion (ROM). If neck motion is decreased or painful, withdraw the athlete from play and obtain cervical radiographs to rule out fracture/dislocation. If symptoms persist for 3-4 weeks following injury, obtain an electromyogram (EMG) to evaluate upper trunk function.[22]
A sprain is defined as an injury to the paraspinal musculotendinous unit. A strain is defined as an injury of the paraspinal muscle itself. An athlete with a sprain or strain usually presents after jamming his/her neck. The pain is localized to the C-spine and limits cervical ROM. Pain and paresthesias do not radiate to the arms. The neural examination is normal, and radiographs are negative for evidence of fracture or dislocation.
Take the player through a series of movements to evaluate the ROM. If the patient has full ROM with no radiation of pain, no paresthesias, and a normal neurologic examination, treat with nonsteroidal anti-inflammatory medications and a soft cervical collar (C-collar) for comfort. Once the pain has resolved, the athlete can return to activity. If the player has limited ROM, protect the neck and remove him or her from activity.
Obtain a radiographic series to include anteroposterior (AP) and lateral flexion/extension views. If a fracture or dislocation is encountered, institute proper immobilization and stabilization. If these radiographs are negative but symptoms persist, obtain an MRI to rule out disk herniation.
Acute disk herniations in football are rare. However, with the acute onset of transient neurologic deficits and negative cervical radiographs, the possibility of a ruptured cervical disk must be considered. Symptoms of herniation vary from radiculopathy to anterior cord syndrome. Anterior cord syndrome occurs with an acute paralysis of the upper, lower, or all 4 extremities. An associated loss of pain and temperature sensation to the level of the lesion occurs.[23] The posterior column vibratory, proprioceptive, and light touch sensations are preserved.
A high degree of clinical suspicion is necessary to avoid missing the diagnosis of a disk injury. If disk injury is suggested, confirm the diagnosis with a CT myelogram or an MRI (see the 4 images below). Once the diagnosis of acute disk herniation with neurologic symptoms is made, an anterior diskectomy with interbody fusion may be necessary.
 T1-weighted MRI of a cervical disk herniation.
T1-weighted MRI of a cervical disk herniation.
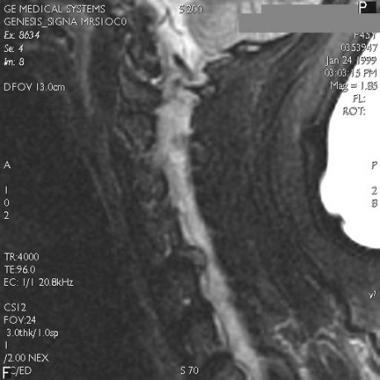 T2-weighted MRI of cervical disk herniation.
T2-weighted MRI of cervical disk herniation.
 Axial CT scan of cervical herniated nucleus pulposus.
Axial CT scan of cervical herniated nucleus pulposus.
 Myelogram of cervical herniated disk. A filling defect is shown.
Myelogram of cervical herniated disk. A filling defect is shown.
In contrast to the rare nature of acute disk herniations in contact sports, disk injuries without frank herniation or neurologic injury can be common and are characterized by chronic changes. Chronic disk changes frequently are seen in athletes who compete in contact sports. Albright studied cervical spine radiographs of 75 University of Iowa freshmen football recruits.[24] The radiographs were obtained after the individuals played high school football but before they played college football. Albright found that 32% had 1 or more of the following conditions:
Albright's findings illustrate that the constant loading of the C-spine in contact sports leads to chronic degeneration. MRI scans of patients with chronic disk injuries reveal a disk bulge with no obvious herniation. Treatment of these patients is conservative, and contact activity should be withheld until the athlete has regained a painless full ROM of the C-spine.
Cervical fractures and dislocations occur when the axial loading forces applied to the C-spine are greater than the yield strength of the vertebral bodies or the supporting ligamentous structures. A spectrum of pathology exists, including the following:
The most important consideration when discussing cervical fractures and dislocations is the concept of stability. Stability, as described by White et al, is the ability of the spine to limit its patterns of displacement during physiologic loads to prevent damage or irritation to the spinal cord and nerve roots.[25] Instability of the adult spine therefore is defined as dysfunction of the posterior elements with more than 3.5 mm displacement (or >20% translation) in the horizontal sagittal plane. See the image below.
 The distance (a) is measured from the posterior-inferior corner of the vertebral body above the allegedly unstable disk space, to the posterior-superior corner of the vertebral body below the allegedly unstable disk space. The distance (b) is the anterior-posterior sagittal-plane diameter of the vertebral body above the allegedly unstable disk space. According to White and Panjabi's outline, evidence of instability exists if the distance (a) is greater than 20% of distance (b). Alternatively, if the linear distance (a) is greater than 3.5 mm, instability is evident. In conclusion: If (a)/(b) x 100 > 20%, or if (a) > 3.5 mm, then instability is evident. In this example (a) = 5.5 mm, (b) = 13.0 mm. 5.5/13 x 100 = 42.3%, and 42.3% > 20%; therefore, instability is evident. Also, (a) = 5.5 mm, which is greater than 3.5 mm; therefore, instability is evident.
The distance (a) is measured from the posterior-inferior corner of the vertebral body above the allegedly unstable disk space, to the posterior-superior corner of the vertebral body below the allegedly unstable disk space. The distance (b) is the anterior-posterior sagittal-plane diameter of the vertebral body above the allegedly unstable disk space. According to White and Panjabi's outline, evidence of instability exists if the distance (a) is greater than 20% of distance (b). Alternatively, if the linear distance (a) is greater than 3.5 mm, instability is evident. In conclusion: If (a)/(b) x 100 > 20%, or if (a) > 3.5 mm, then instability is evident. In this example (a) = 5.5 mm, (b) = 13.0 mm. 5.5/13 x 100 = 42.3%, and 42.3% > 20%; therefore, instability is evident. Also, (a) = 5.5 mm, which is greater than 3.5 mm; therefore, instability is evident.
Instability is also apparent by analyzing the angular measurements between motion segments. Greater than 20° of sagittal plane rotation on flexion/extension films is considered abnormal and potentially unstable. In the acute setting where flexion/extension radiographs are not obtainable, greater than 11° of relative sagittal plane angulation between cervical motion segments on a static lateral C-spine radiograph is considered unstable. See the image below.
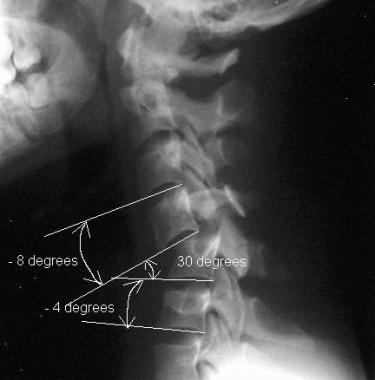 This is a schematic representation of White and Panjabi's description of abnormal angulation. The finding of abnormal angulation greater than 11° between supra-adjacent and subadjacent cervical motion segments on a static lateral cervical spine (C-spine) radiograph is considered unstable. The basic mathematical formula to analyze this is as follows: The angle of the motion segment in question minus the angle of the supra-adjacent segment or the subadjacent motion segment. The difference is less than 11° in the normally stable C-spine. In this image, the formula is illustrated by the following examples: For the supra-adjacent level: 30-(-8) = 38, 38 > 11. For the subadjacent level 30-(-4) = 34, 34 > 11.
This is a schematic representation of White and Panjabi's description of abnormal angulation. The finding of abnormal angulation greater than 11° between supra-adjacent and subadjacent cervical motion segments on a static lateral cervical spine (C-spine) radiograph is considered unstable. The basic mathematical formula to analyze this is as follows: The angle of the motion segment in question minus the angle of the supra-adjacent segment or the subadjacent motion segment. The difference is less than 11° in the normally stable C-spine. In this image, the formula is illustrated by the following examples: For the supra-adjacent level: 30-(-8) = 38, 38 > 11. For the subadjacent level 30-(-4) = 34, 34 > 11.
White and Panjabi's work on cervical instability culminated in the creation of a scoring checklist to serve as an algorithm and an objective assessment of instability. This checklist is illustrated in the White and Panjabi Scoring Cervical Instability Table in the image below.
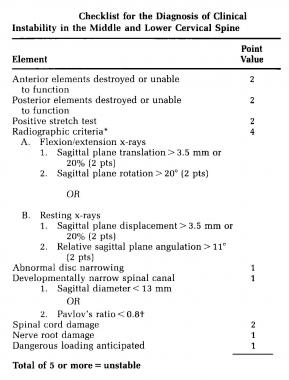 White and Panjabi Scoring Scale for Cervical Instability.
White and Panjabi Scoring Scale for Cervical Instability.
Patients are assessed anatomically, radiographically, neurologically, and physiologically. The patient is graded on each of these criteria, and the grades are added to obtain the final score. A total score of 5 or more is indicative of a patient with an unstable spine.
Subluxation or dislocation without fracture results from disruption of the posterior soft tissue supporting elements. Angulation and anterior translation of the superior vertebrae occurs. No associated fractures exist, and associated neurologic injuries may or may not exist. The diagnosis is made by flexion/extension lateral C-spine radiographs, which show active motion, anterior intervertebral disk space narrowing, and fanning of the spinous processes posteriorly. Obtaining the flexion/extension radiographs in the presence of the treating spine surgeon and in a patient who is awake and communicative is imperative (see the images below).
 Plain radiograph of jumped facets of C4 on C5.
Plain radiograph of jumped facets of C4 on C5.
 Sagittal CT scan of jumped facet.
Sagittal CT scan of jumped facet.
 Sagittal MRI of facet dislocation of C7 on T1.
Sagittal MRI of facet dislocation of C7 on T1.
 Jumped facets.
Jumped facets.
 Jumped facet showing anterior displacement of one vertebra on the adjacent inferior vertebrae.
Jumped facet showing anterior displacement of one vertebra on the adjacent inferior vertebrae.
 Jumped facets with complete anterior displacement of the proximal vertebrae.
Jumped facets with complete anterior displacement of the proximal vertebrae.
An alternative to the flexion/extension radiographs is the use of controlled axial-traction lateral radiographs, also referred to by White as the "stretch test."[26] The stretch test is performed after a standard nontraction lateral C-spine radiograph has been obtained and examined to rule out obvious instability or subluxation.
In the stretch test, the patient is placed supine with the head supported on a roller platform to reduce friction. The head is placed in a traction rig with either Garner-Wells tongs or a head halter, and incremental 10-lb loads of weight are applied. The 10-lb weights are added in the presence of the treating physician. The maximum weight allowed is equivalent to 33% of the patient's body weight.
The physician performs serial neurologic assessments of the patient with each addition of weight. A lateral C-spine radiograph is obtained with each addition of weight. The time interval between weight increments should be at least 5 minutes. The stretch test is considered positive for instability if one of the following situations occurs: (1) the patient sustains a change in neurologic function, (2) on comparison with the pretraction radiograph, there is greater than 1.7 mm of interspace separation of the anterior or posterior elements, or (3) there is greater than 7.5° change in the angle between vertebrae.
The prognosis in patients with subluxation without fracture depends on the degree of displacement. Instability is likely despite nonoperative treatment, and if anterior subluxation is more than 20% of the vertebral body width, treatment should be posterior cervical fusion.
Atlantooccipital dislocations (see the image below) result from high-speed collisions and have never been reported in football. They are described as complete injuries. These injuries usually are fatal secondary to complete respiratory arrest. When this injury is suspected, cervical traction is contraindicated. If the patient survives the injury, treatment is to align the spine and place the patient in a halo vest until C0-C2 fusion can be performed.
 Atlantooccipital dislocation.
Atlantooccipital dislocation.
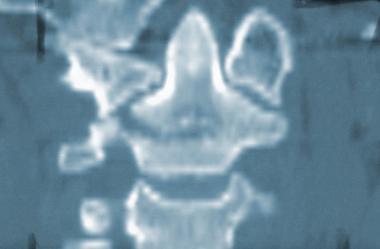
A traumatic rupture of the transverse ligament of the atlas (see the images below) leads to widening of the atlantodens interval and decreased space for the spinal cord.
 Axial CT scan of an increased atlantodens interval.
Axial CT scan of an increased atlantodens interval.
 Sagittal CT scan reconstruction that shows widening of the atlantodens interval.
Sagittal CT scan reconstruction that shows widening of the atlantodens interval.
C1 or atlas fractures (see the images below) usually result from axial loading and are decompressive fractures that rarely result in neurologic deficits. They can be classified as follows:
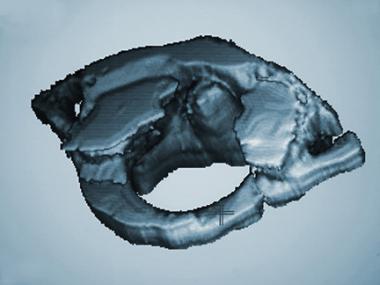 Three-dimensional CT scan of C1.
Three-dimensional CT scan of C1.
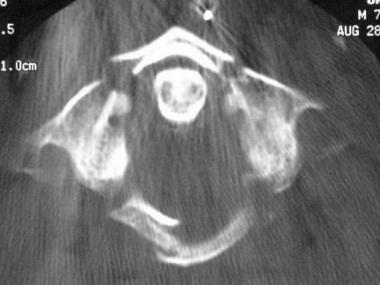 Axial CT scan of a Jefferson fracture.
Axial CT scan of a Jefferson fracture.
See the list below:
All C1 or atlas fractures can be treated with halo vest immobilization until fracture healing occurs.
The 3 types of odontoid fractures are as follows:
 Displaced type II odontoid fracture.
Displaced type II odontoid fracture.
 Anteroposterior view of type III odontoid fracture.
Anteroposterior view of type III odontoid fracture.
 Coronal CT scan of type III odontoid fracture.
Coronal CT scan of type III odontoid fracture.
Traumatic spondylolistheses of C2 also can occur. These fractures also are known as hangman's fractures. They usually are diagnosed on lateral C-spine radiographs. Neurologic injury usually does not occur unless a C2-C3 facet dislocation is present. The 4 types of traumatic spondylolistheses of C2 are as follows:
 Type I C2 traumatic spondylolisthesis. Note the anterior translation but lack of angulation.
Type I C2 traumatic spondylolisthesis. Note the anterior translation but lack of angulation.
 Close-up lateral radiograph of type IIA (Starr-Eismont variant) C2 traumatic spondylolisthesis. Note the significant angulation with minimal translation.
Close-up lateral radiograph of type IIA (Starr-Eismont variant) C2 traumatic spondylolisthesis. Note the significant angulation with minimal translation.
Injuries of the subaxial cervical spine generally are associated with an increased likelihood of neural compression due to a decreasing ratio of canal diameter to cord diameter.
See the list below:
 Avulsion fracture of C7 (the clay shoveler's fracture).
Avulsion fracture of C7 (the clay shoveler's fracture).
 C5 compression fracture.
C5 compression fracture.
 Axial CT scan of C5 compression fracture. Intact middle and posterior columns are shown.
Axial CT scan of C5 compression fracture. Intact middle and posterior columns are shown.
 Plain radiograph of jumped facets of C4 on C5.
Plain radiograph of jumped facets of C4 on C5.
 Sagittal CT scan of jumped facet.
Sagittal CT scan of jumped facet.
 Sagittal MRI of facet dislocation of C7 on T1.
Sagittal MRI of facet dislocation of C7 on T1.
 Jumped facets.
Jumped facets.
 Jumped facet showing anterior displacement of one vertebra on the adjacent inferior vertebrae.
Jumped facet showing anterior displacement of one vertebra on the adjacent inferior vertebrae.
 Jumped facets with complete anterior displacement of the proximal vertebrae.
Jumped facets with complete anterior displacement of the proximal vertebrae.
 Teardrop fracture.
Teardrop fracture.
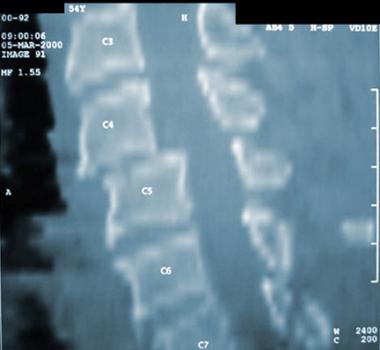
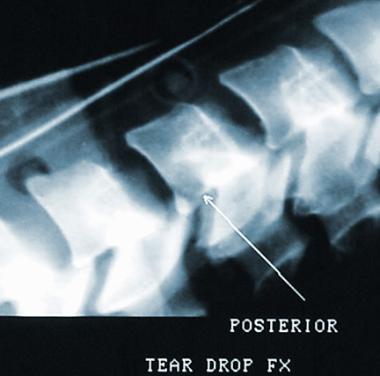 Posterior teardrop fracture.
Posterior teardrop fracture.
The issue of returning to play after a patient sustains a C-spine injury should be based on the risk for further injury, as follows:
Cervical spinal stenosis is defined as the diminution of the anteroposterior diameter of the spinal canal, either as an isolated congenital observation or with disk herniation, degenerative changes, or posttraumatic instability.[29]
Methods of measuring the degree of spinal stenosis continue to evolve with the evolution of imaging technologies. In 1956, Wolfe et al described measuring the space for the cord on plain lateral C-spine radiographs by measuring the distance from the middle of the posterior surface of the vertebral body to the most anterior point on the spinolaminar line for vertebrae C3-7. The normal range was 14.2-23 mm. A measurement of less than 13 mm was considered stenosis. Values obtained by measurement on the lateral plain radiographs could be skewed because of radiographic magnification or variations in radiographic techniques. The actual size of the canal is better assessed by CT scan.
To compensate for these variances in radiographic techniques, Torg and Pavlov described the Torg/Pavlov ratio.[30] This ratio is a measurement of the width of a given vertebral body on the lateral C-spine radiograph divided by the corresponding space allowed for the cord at the same level (see the image below). A value of less than 0.8 was considered to be cervical stenosis and a serious risk factor for neurologic injury in contact sports.
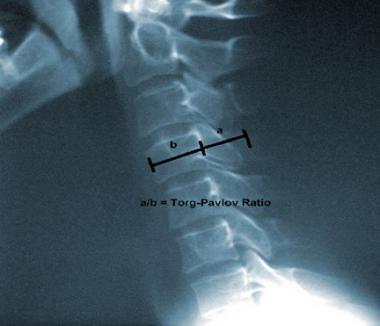 Lateral cervical spine plain radiograph illustrating the Torg/Pavlov ratio.
Lateral cervical spine plain radiograph illustrating the Torg/Pavlov ratio.
Herzog illustrated that the Torg/Pavlov ratio may have resulted in false-positive indications.[31] Herzog reviewed the CT scans of football players with abnormal Torg/Pavlov ratios and found that 70% of players with abnormally small Torg/Pavlov ratios had normal-sized cervical spinal canals.[31] These findings are explained by the fact that football players have abnormally large vertebral bodies. This fact makes the denominator in the Torg/Pavlov ratio larger, and the ratio value is artificially decreased, resulting in a false positive. Additionally, Herzog found no correlation between a Torg/Pavlov ratio of 0.8 and any transient neuropraxia or permanent neurologic deficits. Castro et al, in the American Journal of Sports Medicine, illustrated that cord diameter also varies, and it is the relative difference between the canal size and the cord diameter that creates the clinical condition of stenosis.
Epstein concluded that the presence of a stenotic canal influenced the morbidity and prognosis of a spinal cord injury and that patients with the smallest anterior-posterior canal diameter had the most severe myelopathy following injury.[32] Eismont et al echoed Epstein's conclusions when they looked at 98 patients with C-spine fractures and/or dislocations and found that the sagittal size of the cervical canal correlated with the extent of neurologic injury.[33] They concurred that patients with small diameter canals had more significant neurologic sequelae. Matsura et al found a correlation between the shape of the spinal canal, the central canal diameter, and the predisposition to spinal cord injury.
Cantu advocates the functional definition of spinal stenosis.[34] Functional spinal stenosis is present when the size of the canal is so small that the protective spinal fluid cushion around the cord is obliterated or when the cord is deformed on CT myelogram or MRI. Any athlete with functional cervical stenosis is at increased risk for quadriplegia and should be prohibited from participating in contact sports.
To help establish objective guidelines for return to play following an injury, Watkins et al proposed a point grading system to quantify the patient's clinical situation.[35] This grading system was meant as a guideline for return to play. The physician must consider the entire scenario for each individual player. Watkins et al looked at the following 3 topics and assigned point values according to the player's condition, as follows:
The points tabulated from each of the 3 categories then are added together and compared to the following scoring scale:
These criteria serve as a guide for the team physician; however, the physician should consider each case individually and request the appropriate consultations as needed.[36]
The incidence of catastrophic cervical injuries in sports has significantly decreased over the last 30 years. This decrease is the result of monumental rule changes, such as the ban on spearing in American football, better coaching on contact and tackling techniques, the presence and instruction of athletic trainers at all levels of play, and the improvement in protective gear including helmets and shoulder pads. Unfortunately, when catastrophic neurologic injuries do occur, they are permanent and life changing. The team physician plays a crucial role in the coordination of medical assessment on the playing field, immobilization and transportation to a qualified facility for evaluation and treatment, and decision making regarding return to play following an injury. These decisions should be discussed with the athlete and the athlete's parents, coaches, trainers, and agents. The ultimate decision should be made in the best interest of the patient.[37]
For patient education resources, see the First Aid and Injuries Center as well as Whiplash.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved