

The treatment of lesions of the brachial plexus has changed from shoulder fusion, elbow bone block, and finger tenodesis following World War II to far greater functional restoration by advances in nerve repair and microsurgery.
The natural history of becoming "one-handed" within 2 years has been replaced by early exploration, neurolysis, nerve grafting, neurotization, and free muscle transfers, as well as tendon transfers, for shoulder and elbow function and for wrist or hand prehension. Advances in diagnostic imaging, nerve transfers, electrophysiologic testing, nerve root repair, nerve rootlet replantation, and free muscle transfers have made this a dynamic but highly specialized field.[1, 2, 3]
The image below depicts a clavicle fracture in a patient with a traumatic brachial plexus injury.
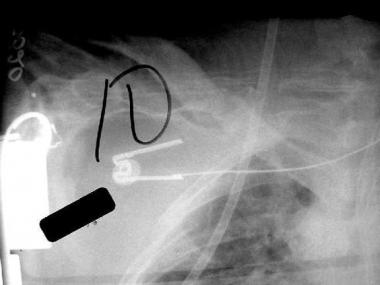 Traumatic brachial plexus injury. Initial anteroposterior chest radiograph of patient involved in accident with 18-wheeled truck. Clavicle fracture observed on initial chest radiograph was important in signaling need for further evaluation of injury because patient was intubated and unresponsive secondary to closed head injury. Scapulothoracic dissociation was suspected on close review of chest CT scan, and brachial plexus injury was noted once patient became responsive.
Traumatic brachial plexus injury. Initial anteroposterior chest radiograph of patient involved in accident with 18-wheeled truck. Clavicle fracture observed on initial chest radiograph was important in signaling need for further evaluation of injury because patient was intubated and unresponsive secondary to closed head injury. Scapulothoracic dissociation was suspected on close review of chest CT scan, and brachial plexus injury was noted once patient became responsive.
See Football Injuries: Slideshow, a Critical Images slideshow, to help diagnose and treat injuries from a football game that can result in minor to severe complications.
NextHigh-energy trauma to the upper extremity and neck can cause a variety of lesions to the brachial plexus. Most common are traction injuries, in which the head and neck are moved away violently from the ipsilateral shoulder; injuries may also be caused by compression between the clavicle and first rib, penetrating injuries, or direct blows. Recognition may be delayed by other injuries, particularly to the spinal cord and head.[4, 5]
Because the topic is a complex one, this article focuses primarily on traction injuries, the most common injuries in adults. Such injuries usually are catastrophic for the affected individual. Loss of useful function of the upper extremity is common, but early repair and reconstruction are providing far greater restoration than was possible a few years ago.
Reliable information on the incidence of traumatic brachial plexus injuries is difficult to find; the exact incidence is not known. Goldie and Coates suggested that 450-500 closed supraclavicular injuries occur each year in the United Kingdom.[6] Young males are disproportionately affected, mostly between 15 and 25 years of age, as in other types of trauma.
On the basis of 18 years of experience with 1068 patients, Narakas developed his rule of "seven seventies," as follows[7] :
The common mechanism for traction injuries of the brachial plexus is violent distraction of the entire forequarter from the rest of the body. These injuries usually result from a motorcycle accident or a high-speed motor vehicle accident. A fall from a significant height may also result in brachial plexus injury, either traction type or from a direct blow; penetrating injuries and low- or high-velocity gunshot wounds also are seen.
In traction-type injuries, the crucial prognostic factor is whether the injury is proximal (preganglionic) or distal (postganglionic) to the dorsal root ganglion. A preganglionic root avulsion means that the cell bodies of the sensory nerves are pulled from the cord, diminishing the possibility of recovery or surgical reconstruction. These are differentiated from distal ruptures — postganglionic stretch injuries — in which cell bodies are still in continuity with their axons.
In traction-type brachial plexus injuries, the head and neck are moved away violently from the ipsilateral shoulder. Upper plexus injuries (C5 and C6) usually predominate if the arm is at the side because the first rib acts as a fulcrum to direct the traction forces preferentially in line with the upper plexus.
When the arm is moved violently and abducted overhead, the lower elements (C8-T1) typically are injured, as the force is directed in line with C7. A lower plexus lesion predominates when the arm is raised because the coracoid acts as a fulcrum in a similar fashion. Lower plexus lesions may be more common, in part, because of the well-formed transverse radicular ligaments that help resist traction forces at C5, C6, and C7; C8 and T1 lack these ligaments.
Traction forces can result in preganglionic or postganglionic injuries. Preganglionic injuries refer to lesions proximal to the dorsal root ganglion, which is in the spinal canal, and foramen. They may be central or direct from the spinal cord or intradural. Preganglionic lesions do not cause wallerian degeneration or neuroma formation because the axons remain in continuity with the cell bodies in the dorsal root ganglion. Postganglionic lesions are defined as any lesions distal to the spinal ganglion and are physiologically similar to other peripheral nerve injuries.
The index of suspicion for a brachial plexus injury is much higher for severe shoulder girdle injuries, particularly motorcycle and motor vehicle accidents. The mechanism of injury should be considered, as these may occur in the setting of polytrauma. Other injuries requiring sedation indicate that detailed follow-up examination of the upper extremity may needed.
The patient may present with the following symptoms:
The standard advanced trauma life support (ATLS) protocol should be followed. Abrasions to the head, helmet, or tip of the shoulder suggest supraclavicular injury. Ptosis (lid droop), enophthalmos (sinking of the eye into the orbit), anhydrosis (dry eye), and miosis (small pupil) or Horner syndrome suggest a complete lower plexus lesion (see the image below), in that the sympathic ganglion for T1 is in close proximity to the brachial plexus.
 Traumatic brachial plexus injury. Patient has ptosis and myosis of his right eye secondary to complete lower brachial plexus lesion.
Traumatic brachial plexus injury. Patient has ptosis and myosis of his right eye secondary to complete lower brachial plexus lesion.
Swelling about the shoulder can be dramatic. Diminished or absent pulses suggest vascular injury, and special consideration should be given to rupture of the subclavian vessels. Clavicle fractures often are palpable. Careful inspection and palpation of the axial skeleton may reveal concomitant injuries. Examine each cervical root individually for motor and sensory function as soon as circumstances allow.
Some special considerations are warranted for the neurologic examination. Sensory examination is extremely important. Deep pressure sensation may be the only clue to continuity in a nerve with no motor function or other sensation (see Table 1 below). Apply full pinch to the nail base and pull the patient's finger outward. Any burning suggests continuity of the tested nerve. When no burning is elicited, these examination findings are less helpful because a neuropraxia can persist for more than 6 months.
Table 1. Deep Pressure Test (Open Table in a new window)
Location of Deep Pressure Test Affected Spinal Nerve Nerve Affected Cord Thumb C6 Median nerve Lateral cord Middle finger C7 Median nerve Lateral cord Little finger C8 Ulnar nerve Medial cord
Examination of wrist and finger sensation and motion with respect to the median, ulnar, and radial nerves may help locate the lesion within the brachial plexus.
Motor examination is also useful (see Table 2 below). Significant variations occur among the spinal nerves within the cord and account for most of the anomalous patterns of innervation. These variations may make identifying the levels involved challenging. In addition, C4 may contribute a branch to the plexus up to 60% of the time. When C4 makes a significant contribution to the plexus, the plexus is called prefixed. A prefixed cord can explain recovery in the distribution of a nerve root clinically presumed to be avulsed.
Table 2. Guide to Motor Testing (Open Table in a new window)
Cervical Root Clinically Relevant Gross Motor Function C5 Shoulder abduction, extension, and external rotation; some elbow flexion C6 Elbow flexion, forearm pronation and supination, some wrist extension C7 Diffuse loss of function in the extremity without complete paralysis of a specific muscle group, elbow extension, consistently supplies the latissimus dorsi C8 Finger extensors, finger flexors, wrist flexors, hand intrinsics T1 Hand intrinsics
When performing the motor examination, keep in mind that most individual muscles have contributions from multiple cervical levels (see the image below).
 Traumatic brachial plexus injury. Human cadaveric dissection of right brachial plexus shows that clavicle and some soft tissues have been resected. Nerve roots are exiting their respective foramina at right-hand border. Uppermost nerve root observed is C5, with C6, C7, and C8 also visible. Cords of plexus can be observed at left-hand margin. Note axillary artery at bottom.
Traumatic brachial plexus injury. Human cadaveric dissection of right brachial plexus shows that clavicle and some soft tissues have been resected. Nerve roots are exiting their respective foramina at right-hand border. Uppermost nerve root observed is C5, with C6, C7, and C8 also visible. Cords of plexus can be observed at left-hand margin. Note axillary artery at bottom.
Elbow flexion and extension determine musculocutaneous and high radial nerve function. Shoulder abduction tests the axillary nerve, which comes off the posterior cord. The posterior cord may also affect deltoid function by the radial nerve. The latissimus dorsi is innervated by the thoracodorsal nerve off the posterior cord, and may be tested by palpation of the muscle while the patient coughs.
Pectoralis muscles can be palpated as the patient adducts the arm against resistance (the medial pectoral nerve to the sternal head comes off the medial cord, the lateral pectoral nerve to the clavicular head comes off the lateral cord). The long thoracic nerve innervates the serratus anterior, and the dorsal scapular nerve innervates the rhomboids; thus, winging of the scapula may help localize the injury.
Formerly, most brachial plexus lesions were treated conservatively. Patients were monitored over 12-18 months for recovery of significant voluntary motor control, and any residual deficit was pronounced permanent. Leffert suggested that after 9-12 months, any residual deficit at the level of the shoulder can be considered permanent.[8] However, recovery of more distal function is sometimes observed more than 1 year after injury. The customary treatments were shoulder fusion, elbow fusion, wrist and finger tenodesis and transhumeral amputation.
The three crucial factors in restoration of upper arm function after brachial plexus injury are as follows:
Open injuries from a sharp object may benefit most from immediate exploration and, if possible, direct, end-to-end repair. With an open injury from a blunt object, a 3- to 4-week delay in repair, after initial debridement and tagging, allows injured nerve ends to demarcate. Low-velocity gunshots injuries may be neurapraxic, and may be observed. High-velocity gunshot injuries need early exploration for significant soft-tissue damage.
Stretch injuries present the most complex issues. Early surgery may preclude opportunities for spontaneous recovery; delayed surgery may allow failure of motor end plates and reinnervation. Suspected avulsions may be explored at 3-6 weeks, and generally, failure of adequate reinnervation may be explored at 3-6 months.
Surgical options include nerve (primary) and soft-tissue (secondary) reconstruction. External neurolysis alone may benefit a nerve in continuity that exhibits a nerve action potential (NAP). Postganglionic neuromas or ruptures may benefit from nerve grafting. From an overall perspective, such grafts include C5 for shoulder abduction, C6 for elbow flexion, and C7 for elbow and wrist extension.
Nerve transfers (neurotization) can be performed to accelerate recovery from preganglionic injuries.[9] Such procedures, performed ideally within 6 months, reduce time to reinnervation by reducing the distance to the site of the nerve injury.
Sources for transfer include the spinal accessory nerve, intercostal nerves, and the medial pectoral nerve.[10, 11] These improve shoulder abduction and external rotation in the common but devastating high plexus injuries (C5, C6).[12] The Oberlin transfer uses a fascicle of a functioning ulnar nerve, but the median nerve or others may also be used in specific cases.
Significant recovery after nerve grafting can take more than 18 months, and maintaining joint mobility, minimizing edema, and treating deafferentation pain during this period can make postoperative care challenging.
The age of the patient also is important. The ability of nerve transfers to restore functional strength decreases dramatically with patient age. Therefore, many of the surgical options are reserved for younger patients.
The brachial plexus is formed from the spinal nerves or roots, the coalescence of the ventral (motor) and the dorsal (sensory) rootlets as they pass through the spinal foramen. The dorsal root ganglion contains the cell bodies of the sensory nerves; the cell bodies for the ventral nerves lie within the spinal cord.
Typically, the brachial plexus is formed from C5-T1; in some cases with there is a contribution from C4 (prefixed, 28-62%) or T2 (postfixed, 16-73%). All nerve supply to the upper extremity passes through this plexus. The brachial plexus starts at the scalenes, courses under the clavicle, and ends at the axilla. It is typically composed of five roots, three trunks, six divisions (two from each trunk), three cords, and terminal branches.
The five roots are named by the level with which they correspond. The C5-7 roots give off branches to form the long thoracic nerve, and the C5 root gives branches to form the dorsal scapular nerve. C5 and C6 gives branches to form the superior trunk, C7 the middle trunk, and C8 and T1 the inferior trunk.
Each trunk has two divisions: one division of each of the trunks forms the posterior cord; the anterior division of the superior trunk and the anterior division of the middle trunk form the lateral cord. The anterior division of the inferior trunk forms the medial cord. The medial, lateral, and posterior cord designations describe their relationship to the axillary artery.
The superior trunk gives off the suprascapular nerve and a nerve to the subclavius. The posterior cord has the upper and lower subscapular nerves, with the thoracodorsal nerve between them. The lateral pectoral nerve emanates from the lateral cord, and the medial pectoral nerve from the medial cord, but with a connection between the pectoral nerves. The posterior cord then becomes the axillary and radial nerves.
The lateral cord continues as the musculocutaneous nerve; a branch from the medial and lateral cords becomes the median nerve; and a branch from the lateral branch joins the medial cord continuation as the ulnar nerve, after the medial cord gives off the medial brachial cutaneous and the medial antebrachial cutaneous nerves.
The cords and branches are distal to the clavicle; the roots and trunks proximal. The plexus lies in close proximity to the axillary artery, which exits between the anterior and middle scalenes. Knowledge of this anatomy may allow localization of lesions from the physical examination.
Many different approaches to the brachial plexus have been used. Surgeons' preferences are largely shaped by training and by the goals of a particular procedure. In any approach, the clavicle can be a barrier to visualization.
Millesi described an approach using three anterior incisions with the patient in the supine position.[13] He makes a sagittal incision on the lower neck and two transverse incisions more distally, following skin tension lines. By moving the clavicle and looking at the plexus from both a cephalad and a caudad direction, he is able to visualize upper, middle, and lower trunks of the brachial plexus and avoid osteotomy of the clavicle. The spinal nerves of the upper plexus can also be visualized with this approach.
Contraindications to surgery include the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved