

Hand injuries are common and account for 5-10% of emergency department (ED) visits nationwide. The complexity of the hand and the similarities in clinical presentation of different injuries make understanding of hand anatomy and function, good physical examination skills, and knowledge of indications for treatment indispensable for the emergency physician.
Thorough knowledge of the anatomy and functions of the hand is required for proper diagnosis and treatment. Use of proper terminology prevents confusion that may compromise the care of patients with hand injuries. The following is a brief review of standard terminology and key anatomic structures.
Motion and position: Standard terminology also applies to motions and positions of the hand and digits.
Surface anatomy: Three creases are present on the palmar surface of the digits. The distal and middle palmar creases correspond to the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints, respectively. The proximal digital palmar crease does not overlie a joint as the MCP is more proximal. The long thenar crease partially encircles the thenar eminence and overlies the metacarpophalangeal (MCP) joint.
Bony anatomy: The wrist is composed of 8 carpal bones arranged in 2 rows of 4. The flexor retinaculum together with the carpal bones forms the carpal tunnel. The median nerve passes through the carpal tunnel with the tendons of the flexor digitorum profundus and superficialis. The ulnar nerve enters the hand passing between the hook of the hamate bone and the pisiform bone in the Guyon canal.
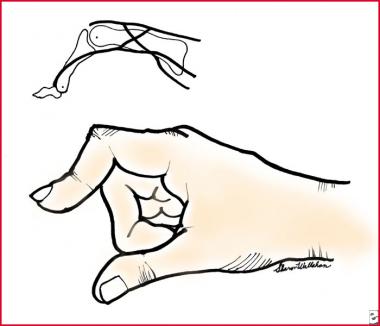
The metacarpal bones articulate with the wrist at the carpometacarpal (CMC) joints. The metacarpophalangeal (MCP) joints are formed by the articulation of the metacarpal bones with the proximal phalanges (see the image below). The heads of the metacarpals form the knuckles, which are seen dorsally with the closed fist. The thumb has only 1 interphalangeal (IP) joint, while the rest of the digits have proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints.
 Metacarpophalangeal joints of the digits
Metacarpophalangeal joints of the digits
Each of the MCP, PIP, and DIP joints has collateral ligaments, which provide lateral stability, and a volar plate, which prevents hyperextension. The volar plate is damaged frequently in subluxation and dislocation injuries.
Blood supply: The blood supply to the hand is derived from the ulnar and radial arteries, which form the superficial and deep palmar arterial arches by anastomosis. In the absence of vascular disease, either artery alone is sufficient to perfuse the entire hand in most of the population.
Extrinsic and intrinsic muscles: The muscles of the hand are designated intrinsic or extrinsic. Extrinsic muscle bellies are in the forearm and their tendons insert into the hand, while intrinsic muscles both arise in and insert in the hand. The muscles of the hand and digits also are named according to their function as either flexors or extensors.
Forearm flexors: The forearm flexors are extrinsic muscles of the hand. These muscles arise from the medial epicondyle of the humerus and include the following:
The tendons of flexor carpi radialis (FCR), palmaris longus, and flexor carpi ulnaris (FCU) are visible in the forearm (see the image below). The palmaris longus is absent in about 14% of the population. The median nerve lies between the palmaris longus and the flexor carpi radialis (to the ulnar side of the FCR). The flexor carpi ulnaris is a good landmark to locate the ulnar nerve and artery, which lie to the radial side of the FCU.
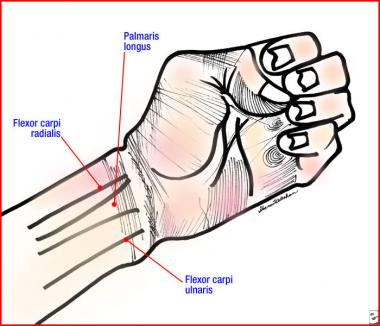 Volar tendons at the wrist. These can be used as landmarks for injections.
Volar tendons at the wrist. These can be used as landmarks for injections.
Flexion of the fingers is controlled by the flexor digitorum profundus and superficialis muscles. Both of the finger flexors lie on the ulnar side of the wrist with the median and ulnar nerves and the ulnar artery. The flexor carpi ulnaris and radialis flex the wrist when acting together and cause deviation to their respective active sides when contracting separately.
Intrinsic muscles of the hand: Branches of the median and ulnar nerves innervate all the intrinsic muscles of the hand. They can be divided into 3 groups as follows: thenar (thumb), hypothenar (little finger), and lumbricals.
The thenar eminence is formed by the extensor pollicis brevis and the 3 short thenar muscles: the abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis. These muscles have short tendons that insert onto the proximal phalanx of the thumb. They are innervated by the recurrent branch of the median nerve. The superficial location of this branch renders it vulnerable to seemingly trivial trauma to the thenar eminence.
Forearm extensors: Eleven muscles extend the wrist, hand, and digits (see the image below). The forearm extensors pass into the hand in 6 compartments. All forearm extensors arise from the lateral epicondyle of the humerus. They are innervated by the radial nerve.
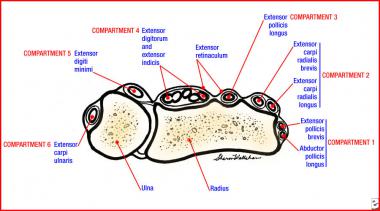 Sagittal section of extensor compartments
Sagittal section of extensor compartments
Innervation: The median, ulnar, and radial nerves supply all of the sensory and motor innervation to the hand. The superficial volar and dorsal distributions of the sensory nerves are shown in the images below. The median nerve enters the hand via the carpal tunnel and often is involved in carpal tunnel syndrome. The median nerve sends motor fibers to the 3 short thenar muscles and the first and second lumbricals. The ulnar nerve sends motor fibers to the hypothenar muscles, the ulnar 2 lumbricals, the adductor pollicis, and all of the interosseous muscles. The radial nerve sends no motor branches to the intrinsic muscles of the hand.
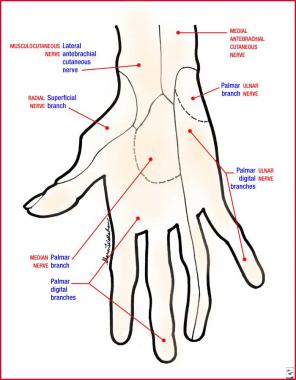 Superficial volar sensation of the hand
Superficial volar sensation of the hand
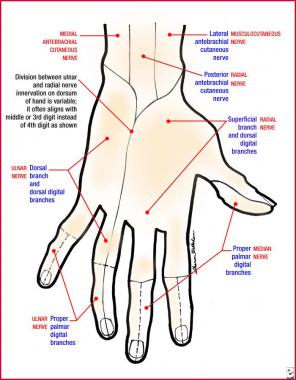 Superficial dorsal sensation of the hand
Next
Superficial dorsal sensation of the hand
Next
The pathophysiology of soft tissue injuries of the hand is diverse. The most common mechanisms of injury are blunt trauma (eg, crush injury, contusions, abrasions), laceration, avulsion, ring avulsion, and burns. Besides skin and superficial tissues, the many muscles, ligaments, and tendons of the hand are vulnerable to injury, as are the nerves and blood vessels that supply these structures. Damage to these structures may create permanent functional and/or sensory deficits specific to the site of injury.[1, 2, 3]
Blunt, penetrating, and crush injuries to the hand result in nerve damage.[4] Nerve injury is divided into 3 types, as follows:
DIP: The DIP joint is stabilized not only by collateral ligaments but by adjacent flexor and extensor tendons, making dislocations of this joint uncommon. If dislocation does occur, it usually is directed dorsally and often is associated with an open wound. DIP joint dislocations are detected easily by physical examination.
PIP: The ligaments of the PIP joints are the most commonly injured in the hand. Dorsal dislocations are the most common and usually are the result of a blow to the extended digit, causing a combination of axial loading and dorsal deviation. Volar dislocations are uncommon because the joint does not resist motion in this direction. Lateral dislocation is the result of a tangential load applied to the extended digit that ruptures a collateral ligament and disrupts the volar plate. Ulnar deviation, with rupture of the radial collateral ligament, is more common than radial deviation.
MCP: Dislocation of the MCP joint is uncommon, but when it occurs deviation is usually dorsal. The common mechanism of injury is the application of a dorsally directed force that is sufficient to rupture the volar plate. Dorsal dislocations in 60-90° of hyperextension and without intervening soft tissue are simple dislocations. Complex dislocations have the volar plate entrapped between the metacarpal and the proximal phalanx. Complex dislocations are less striking in their clinical presentation but are more serious injuries.
Thumb: The IP joint of the thumb is very stable and seldom injured. Dislocations usually are dorsal and often open. The MCP joint of the thumb is one of the most frequently injured joints. Injury most commonly is caused by hyperextension force sufficient to rupture the volar plate and cause dorsal dislocation. As in MCP joints of the other digits, dorsal dislocation of the MCP joint may be a simple subluxation or complex dislocation. The complex dislocation is complicated by entrapment of the proximal phalanx.
Joints of the digits are stabilized by the combination of collateral ligaments and the volar plate. Stretching or partial tearing of the ligaments results in a sprain. The volar plate may be injured alone or in combination with the collateral ligaments. The common mechanism for an isolated volar plate injury is hyperextension during an axial load. Pain location is a good indicator of the site of injury. For example, lateral pain suggests collateral ligament injury, whereas pain on the palmar surface of the joint suggests volar plate injury. Loss of stability more commonly is associated with joint dislocation.
Sprains of the PIP and MCP joints produce pain and swelling but may lead to little or no instability. They are classified as first, second, or third degree. If the joint does not open at all but has pain with stressing of a ligament, the injury is first degree. A joint that is opened slightly in the ulnar or radial direction is defined as having a second-degree injury. This finding suggests a unilateral collateral ligament tear. A joint that is opened by at least 3-5 mm must have damage to at least 2 of the 3 structures stabilizing the joint (ie, volar plate, 2 collateral ligaments). This is referred to as a third-degree sprain or an unstable joint. Serious ligamentous injuries occur frequently and often are misdiagnosed because a mild sprain may have a similar presentation. Sequelae from missed ligamentous injuries range from chronically painful to chronically unstable or deformed joints.
Sprains of the MCP joint are rare because of the anatomy of the joint, the laxity of the collateral ligaments, and the protection afforded the joints by surrounding structures. Hyperextension of the extended digit is the most common mechanism causing sprains. Diagnosis is indicated by a stable but painful edematous joint.
The ability to hold objects between the thumb and 4 fingers is an essential function of the hand and depends upon an intact ulnar collateral ligament (UCL). Injury to the UCL is known as the gamekeeper's thumb or skier's thumb. This is because Scottish gamekeepers frequently damaged their UCLs killing game. The head of a small animal was placed between the thumb and index finger and a hyperextension/longitudinal traction force applied to the animal's cervical spinal cord by abruptly yanking the lower extremities. In a certain percentage of these procedures, the UCL of the gamekeeper was disrupted.
In modern times, skiing is the activity that most often causes UCL injury. However, a history of a missed punch, a fall onto the thumb, or the forceful removal of an object from the flexed hand also should be considered suggestive of UCL injury.
The common mechanism of injury is the forceful abduction of the thumb. Any patient with pain in the distribution of the UCL or inability to forcefully oppose the thumb has an injury of the UCL until proven otherwise.
Rupture of the radial collateral ligament of the thumb is much less common than UCL rupture. The mechanism of injury is forceful adduction of the thumb in any position.
The extensor tendons' superficial location predisposes them to injury from seemingly trivial lacerations as well as avulsions, crushes, and burns.[2, 3, 5, 6] Flexor tendon injuries can be caused by lacerations. Tendon injuries also may be sustained as the result of forced hyperextension or forced flexion of an extended digit. Injuries may include complete or partial transection, avulsion, or maceration. Whenever a tendon is damaged, particularly with an open injury, the vessels and nerves that are in close proximity may be injured.[7, 8]
Understanding that a tendon may be 70-90% lacerated and still functional is critical. Damage to these tendons may result in such findings as boutonnière deformity and mallet finger (see the images below).[9, 5]
 Boutonnière deformity due to closed central tendon rupture
Boutonnière deformity due to closed central tendon rupture
 Boutonnière deformity
Boutonnière deformity
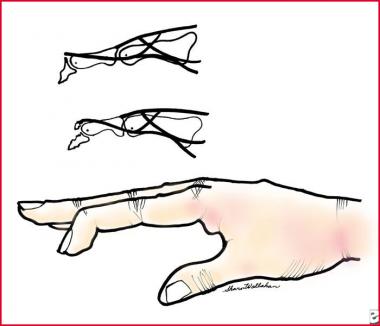 Mallet finger due to loss of central extensor tendon to the distal phalanx
Mallet finger due to loss of central extensor tendon to the distal phalanx
Soft tissue injuries of the hand rarely are life threatening. However, the high incidence of disability from chronically painful or unstable joints is reflected by the fact that hand derangements account for 9% of all worker compensation claims.
The costs for treating these injuries are considerable and include not only the direct costs of repair but also the indirect costs borne by the patient, his or her family, and society. These indirect costs include, for example, time off from work and costs incurred while seeking care.[10]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved