

Distal humerus fractures in adults are relatively uncommon injuries, representing only about 3% of all fractures in adults. In a study of 4536 consecutive fractures in adults seen in the Massachusetts General Hospital emergency department, only 0.31% were supracondylar (bicolumn) fractures of the distal humerus. Although these injuries are relatively rare, most orthopedic surgeons are called upon to evaluate and treat patients with these injuries and, therefore, must be equipped to achieve optimal outcomes.[1, 2, 3]
We live in a society with a growing elderly population and a young population in which extreme sports and high-speed motor transportation are popular; therefore, the incidence of these fractures is likely to increase. In young adults, most distal humerus fractures occur from high-energy trauma, sideswipe injuries, motor vehicle accidents, falls from heights, and gunshot wounds. In elderly persons with more osteoporotic bone, most of these injuries occur from falls.
Numerous classification schemes have been devised to categorize and discuss supracondylar fractures. In 1936, Reich originally classified supracondylar fractures into T and Y variations.[4] In 1969, Riseborough and Raidin described four categories based on degree of displacement, comminution, and rotation.[5] As surgeons became more adept at surgical reduction and internal fixation, the Arbeitsgemeinschaft für Osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) group described a classification based on fracture pattern and degree of comminution.
AO-ASIF type A fractures are extra-articular fractures and are further subclassified as follows:
AO-ASIF type B fractures are unicondylar fractures and are further subclassified as follows:
AO-ASIF type C fractures are bicondylar fractures and are further subclassified as follows:
This classification remains somewhat deficient in describing the mechanically important concept of the medial and lateral columns and their fracture involvement. It also is somewhat deficient in describing the level through which the fracture occurs in each column and related important surgical considerations. Because of these limitations, this author believes that the classification of bicolumn fractures of the distal humerus introduced by Mehne and Matta proves useful in planning bicolumn surgical fixation.
The classification of Mehne and Matta describes the specific characteristics of bicolumn fractures and allows for better preoperative planning.[6] The classification is as follows:
Although the medial and lateral lambda fractures are not technically bicolumn fractures, they are included in this classification because they require similar operative fixation techniques (see the image below).
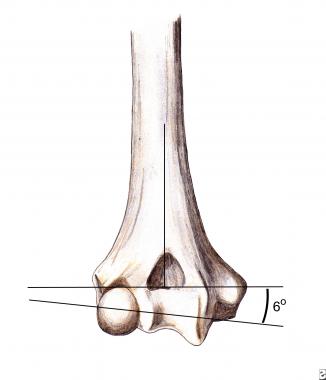 Supracondylar humerus fractures: anatomy. Trochlea rests in 6-8º valgus in relation to humeral shaft.
Next
Supracondylar humerus fractures: anatomy. Trochlea rests in 6-8º valgus in relation to humeral shaft.
Next
Surgical treatment of supracondylar fractures has evolved significantly over the past few decades. In the 1960s and 1970s, most surgeons condemned surgical treatment because of high failure rates with loss of fixation, nonunion, and elbow stiffness. In the 1970s, treatment began to shift from casting and the "bag of bones" technique to surgical intervention with limited internal fixation. Again, results generally were poor owing to lack of adequate stabilization for early motion.
In the early 1980s, the Arbeitsgemeinschaft für Osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) group reported good and excellent results in 27 of 39 patients with comminuted fractures of the distal humerus. These by far were the best results reported in the treatment of these difficult fractures at that time. This led to an increased enthusiasm for surgical reduction and fixation. Additional surgical approaches were developed, along with more versatile fixation hardware, leading to improved surgical results.
The "bag of bones" treatment was used when bone quality or fracture pattern was not sufficient to gain stable fixation. This led to generally poor and unpredictable results. This approach has now largely been replaced by total elbow arthroplasty, allowing improved and more predictable results.
Single-column fractures are relatively rare and account for only 3-5% of distal humerus fractures. Lateral column fractures are more common than medial column fractures. These fractures represent the distal extent of the respective column, including a portion of the articular surface. These are described as high or low, depending on the proximal extent of the fracture line and the extent of joint surface involvement. Milch previously described these as medial or lateral condyle fractures.[7]
Bicolumn fractures are far more common distal humerus fractures. In some reports, these account for as many as 70% of distal humerus fractures in adults. These fractures involve disruption of both the medial and lateral columns, thus disrupting the humeral triangle and resulting in disassociation of the articular surface from the humeral shaft. Successful treatment is most challenging in these fractures.
The mechanism by which these fractures occur has been a topic of debate. Historically, the mechanism has been accepted to be an axial load on the elbow, with the olecranon acting as a wedge splitting the medial and lateral columns of the distal humerus. However, mechanical studies performed on cadavers have shown that supracondylar (bicolumn) fractures are more likely to be produced with the elbow flexed beyond 90°. The fracture pattern is related to the degree of elbow flexion and the direction and magnitude of the force applied.
The clinical presentation is that of a painful swollen elbow that the patient is hesitant to move. The elbow may appear angulated and the upper extremity shortened. Some series report that open wounds are present in as many as 30% of these fractures. Patient history includes a high-energy trauma or significant fall. Evaluate adjacent joints for associated injuries.
Neurovascular status must be carefully evaluated and monitored. Owing to the close proximity of the neurovascular structures, injury is not uncommon. If a deficiency is noted, carefully evaluate and document when it first became apparent, the degree of involvement, and possible progression. If it first appeared following manipulation or splint placement, consider remanipulation; if the deficiency does not resolve, urgently explore to evaluate possible nerve entrapment. Neurapraxias are not uncommon and generally resolve with restoration of normal alignment and lengths. In the author's experience, resolution has occurred up to 18 months after injury.
Radiographic evaluations should include standard anteroposterior (AP) and lateral films. With comminuted bicolumn fractures (type C3 in the Arbeitsgemeinschaft für Osteosynthesefragen–Association for the Study of Internal Fixation [AO-ASIF] classification), repeat films following initial reduction or with longitudinal traction maintained often prove helpful to further define articular fracture fragments. For complicated fractures, computed tomography (CT) also can be helpful with regard to surgical planning.
If vascular compromise is evident, obtain emergency arteriograms. If arterial disruption is present, obtain a vascular surgery consultation followed by immediate open reduction and internal fixation to provide skeletal stability and support of vascular reconstruction.
The main goals of surgical treatment of supracondylar humerus fractures are to prevent further injury, to restore normal anatomy, and to provide an optimal environment for healing. If these goals are met, the patient will have the best possibility of regaining optimal function. If any surgical treatment of the distal humerus is undertaken, the goals also must include affording adequate stability to allow immediate range of motion.
Long-term results after surgical treatment of these complex fractures have improved, largely because of improved surgical technique in gaining stability to permit early motion. Adult elbows after such an injury are not tolerant of prolonged immobilization, and if arthrofibrosis occurs, regaining function becomes extremely difficult if not impossible. Therefore, the goal of surgery is to stabilize to mobilize.
Fractures in which stable reduction could not be obtained were previously treated with the "bag of bones" technique. In this technique, early range of motion was allowed, without attempted reduction and fixation. This led to generally poor results, with limited motion, pain due to noncongruent joint surfaces and nonunions, and cosmetic deformity. Because of these poor results, this treatment has now been largely replaced by total elbow arthroplasty.[8]
For proper evaluation, planning, and execution of surgical treatment of these fractures, the surgeon must have a solid understanding of the relevant anatomy from both a functional and a surgical perspective. (See the images below.)
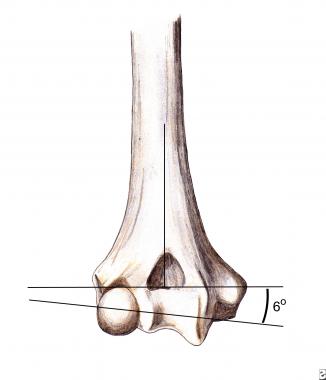 Supracondylar humerus fractures: anatomy. Trochlea rests in 6-8º valgus in relation to humeral shaft.
Supracondylar humerus fractures: anatomy. Trochlea rests in 6-8º valgus in relation to humeral shaft.
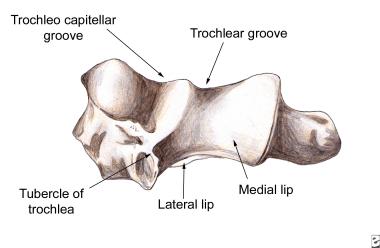 Supracondylar humerus fractures: anatomy. When viewed on end, trochlea resembles spool.
Supracondylar humerus fractures: anatomy. When viewed on end, trochlea resembles spool.
Functionally, the elbow joint behaves as a constrained hinge. The olecranon of the ulna articulates around the trochlea of the humerus. The trochlea normally is tilted in 4° of valgus in males and 8° of valgus in females, thus creating the carrying angle of the elbow. The trochlea also is externally rotated 3-8° from a line connecting the medial and lateral epicondyles, resulting in external rotation of the arm when the elbow is flexed 90°. The images below depict relevant anatomy.
A second plane of motion occurs with the elbow joint in supination and the forearm in pronation; this range of motion is allowed by the radial head articulation with the capitellum and the ulnar notch.
The surgical anatomy closely mirrors the functional anatomy. For stable elbow motion, the trochlea must be restored to its normal position, acting as a tie rod between the medial and lateral columns of the distal humerus. This forms the triangle of the distal humerus, which is crucial for stable elbow function (see the image below).
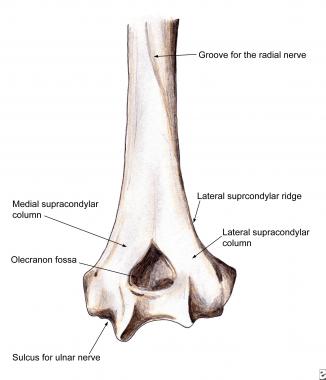 Supracondylar humerus fractures: anatomy. Note medial and lateral columns, connected by trochlea, thus forming triangle of distal humerus. Also note location of sulcus for ulnar nerve in relation to placement of medial plate, as well as location of radial nerve sulcus in relation to proximal placement of plates.
Supracondylar humerus fractures: anatomy. Note medial and lateral columns, connected by trochlea, thus forming triangle of distal humerus. Also note location of sulcus for ulnar nerve in relation to placement of medial plate, as well as location of radial nerve sulcus in relation to proximal placement of plates.
Both columns must be securely attached to the trochlea. Make every attempt to restore the proper valgus tilt and external rotation of the trochlea so as to achieve stability, full motion, and a normal carrying angle. The coronoid is important to elbow stability and should be reduced and fixated if displaced.
The olecranon fossa, a very thin wafer of bone, does not require restoration if badly comminuted. If the medial and lateral columns can be securely fixated to the trochlea, early motion should be tolerated. The medial column diverges from the humeral shaft at approximately 45°, continues, and ends in the medial epicondyle. Because nothing articulates with the anteromedial epicondyle, the entire surface is available for internal fixation hardware. Be careful to protect and transfer the ulnar nerve anteriorly.
The lateral column diverges from the humeral shaft at approximately 20° and is largely cortical bone with a broad flat posterior surface; thus, it is ideal for plate placement. At the posterior capitellum, cancellous screws must be used to avoid interrupting the anterior capitellar cartilage. Biomechanical studies have demonstrated the strongest construct of fixation of bicondylar fractures to be a direct medial plate and posterolateral plate with screws directed at 90° angles. This provides the varus and valgus rotational stability to the construct, thus allowing early range of motion.
Contraindications to surgical treatment with open reduction and internal fixation include severe osteopenia, making adequate stabilization impossible. An insensate or avascular arm, which cannot be restored, makes any surgical treatment short of amputation futile. This occurs in severe sideswipes, crush, or avulsion-type injuries.
As a general rule, attempts should be made to salvage the upper extremity; even a somewhat limited arm, if sensate, is functionally better than an upper-extremity prosthesis. Severe contamination or soft-tissue injury must be dealt with before final stabilization in order to provide an optimal environment for healing and lessen the likelihood of infection.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved