

The procedure for evaluation and management of open fractures is best described as a set of principles that has evolved over time, often in relation to advances in wartime care of military personnel. These principles involve both initial management and subsequent surgical intervention.[1, 2, 3]
The first step is accurate diagnosis and documentation of the mechanism of injury. Appropriate coverage of the wound and splinting of the fracture are performed in conjunction with initiation of appropriate antibiotic therapy and tetanus prophylaxis. Urgent surgical intervention typically follows and involves both soft tissue and bone management. Adjuncts to the care of open fractures have evolved and often involve delivery of antibiotics or metabolically important substances to the local fracture environment.
These principles are generally well established and accepted across the orthopedic community, but in some respects, controversy still exists regarding the details.
Open fractures pose some unique risks beyond those encountered with similar closed fractures that may occur with similar amounts of force. The greatest problem is the risk of infection. Diaphyseal bone loss in excess of 3 cm presents a complex set of problems as well. If the open fracture was caused by penetrating trauma, direct injury to major neurovascular structures may be more likely, thereby affecting the prognosis for limb function.
The risk of a fracture being open is related to the amount of soft-tissue coverage in that region of the body and to the amount of energy imparted to that region. For example, the tibia has a long medial aspect that is subcutaneous, and therefore, it is “easier” for trauma to the lower leg to expose the bone and fracture site. Conversely, the femur is surrounded by thick muscle layers circumferentially and, therefore, is less likely to be exposed after a similar amount of force to the thigh.
For more information, see the following topics:
Open fractures occur in many ways, and the location and severity of the injury are directly related to the location and magnitude of the force applied to the body. Clearly, this involves a broad spectrum of clinical scenarios.
In the most benign form, an open fracture may involve a very small wound caused by a sharp bone spike, creating a small, minimally contaminated hole in the overlying skin. The opposite end of the spectrum may involve high-velocity gunshot wounds, vehicular trauma, or industrial accidents with associated tissue crushing and devitalization.
Direct inoculation of the tissue is a basic issue in the pathophysiology of open fracture management. Furthermore, bacteria can colonize wounds at later stages of care, being introduced into the wound at subsequent dressing changes or repeat debridements prior to definitive wound closure. Gustilo and Anderson reported that 50.7% of their 158 patients had a positive wound culture upon initial evaluation.[4] Another 31 patients that were initially culture negative had a subsequent positive culture at the time of their definitive closure.
Because of the identification and sensitivity of the invading organisms, a first-generation cephalosporin and aminoglycosides have become the most common choices for initiation of antibiotic therapy after open fracture.
Devitalized tissue results from the energy imparted to the body. A crushing injury can impair the local immune response, with local ischemia playing a large role in this process. Ischemia may also occur by direct trauma to the large vessels and/or microcirculation. Important indirect causes of ischemia include increased myofascial compartment pressures, increased vascular permeability, and the use of vasoconstrictive medications during resuscitation.
Virtually all open fractures must be considered for operative intervention. The introduction of bacteria and soft-tissue compromise associated with even “minor” open fractures mandate appropriate presurgical and surgical management to minimize the risk of clinically important complications.[5, 6]
Perhaps the only absolute contraindication for operative management of an open fracture arises if the patient is in such critical condition that any operative intervention could lead to further deterioration; however, there is no evidence from randomized controlled trials to support this concept. Even the patient in extremis may benefit from wound irrigation and sterile application of traction or external fixation in the trauma bay or trauma care unit until a formal irrigation and debridement can be undertaken in the operating room.
Laboratory tests are typically not directly important for the acute care of an open fracture. However, many patients with open fractures will have other injuries that require appropriate laboratory investigation, and Advanced Trauma Life Support (ATLS) guidelines should be followed for workup of the traumatized patient.[7]
Acute bacterial culture of open fracture wounds, before or shortly after initial debridement, is of little clinical utility.[8] Organisms isolated in the acute phase of treatment do not correlate well with clinical infections that result from open fractures. Therefore, the routine use of cultures at this stage of care is of little benefit to the patient and is not cost-effective.
Basic orthogonal radiographs (typically, anteroposterior and lateral projections) are taken of the injured extremity. The images should include the joint proximal and distal to the area of injury. Oblique images can be used to obtain further information, as needed. Evaluation of skeletally immature patients is often facilitated by use of comparison views of the contralateral extremity or joint involved. (See the images below.)
 An open midfoot fracture with bone loss at the base of the first metatarsal, including approximately 66% of the joint surface.
An open midfoot fracture with bone loss at the base of the first metatarsal, including approximately 66% of the joint surface.
 The foot was cared for with serial debridement and temporary pinning of the midfoot to preserve alignment with minimal additional surgical trauma.
The foot was cared for with serial debridement and temporary pinning of the midfoot to preserve alignment with minimal additional surgical trauma.
 An antibiotic-impregnated cement spacer was placed in the bone void, and 12 weeks later, after the pins had already been removed, a midfoot fusion was performed.
An antibiotic-impregnated cement spacer was placed in the bone void, and 12 weeks later, after the pins had already been removed, a midfoot fusion was performed.
 Intraoperative image of the midfoot fusion. The cement spacer has been replaced by autologous bone graft from the iliac crest.
Intraoperative image of the midfoot fusion. The cement spacer has been replaced by autologous bone graft from the iliac crest.
Computed tomography (CT) and magnetic resonance imaging (MRI) provide further detail of bone and soft-tissue injury, but they are often not immediately needed for the acute management of an open fracture. They tend to be most useful in the management of complex periarticular injuries.
The use of ultrasonography to assess tissue perfusion, myofascial compartment pressure monitors, and perhaps magnetic resonance angiography (MRA) or enhanced CT imaging of the soft-tissue elements of the extremity are all current areas of intense research and should provide increased levels of predictive data when validated.
Internationally, for adults and pediatric patients, the modified Gustilo-Anderson classification is widely used.[4] Their initial description was published in 1976, as follows:
The description of type III fractures was subsequently further refined and described by Gustilo et al in 1984,[9] as follows:
It is important to note that the severity of the injury may not be fully appreciated at the time of initial evaluation, and therefore, classification should be based on the intraoperative findings.
The Orthopaedic Trauma Association (OTA) published a fracture and dislocation classification compendium, according to which open fractures are categorized on the basis of five main variables, as follows.[10]
Skin injury:
Muscle injury:
Arterial injury:
Contamination:
Bone loss:
To date, relatively few studies have been done comparing the Gustilo-Anderson and OTA classification systems with regard to prediction of treatment outcomes (eg, infection, limb amputation, need for soft-tissue coverage, or limb salvage). In a retrospective study aimed at examining this question, Hao et al found the OTA system to be better than the Gustilo-Anderson system at predicting postoperative complications and treatment outcomes in patients with open long-bone fractures.[11]
Patzakis et al described the value of acute systemic antibiotic use for open fractures.[12] In a later review article, Patzakis and Zalavras pointed out that the administration of antibiotics is best considered therapeutic, not prophylactic, because of the high risk of infection in the absence of antibiotics.[13]
Although debate still surrounds some aspects of antibiotic administration for open fractures, the following generalizations can be made:
The emergence of various antibiotic-resistant organisms and the development of alternative regimens of antibiotics for use in open fractures have not yet been sufficiently well studied.
Immunization and prophylaxis against tetanus deserve specific consideration. Tetanus is caused by infection from Clostridium tetani, which is an anaerobic bacterium commonly found in soil, and the toxins produced by the bacteria lead to severe and potentially life-threatening muscular spasm. Immunization of civilians became widespread after successful use of heat-inactivated toxin during World War II.[14]
On the basis of a review of various sources, Rhee et al made the following recommendations regarding tetanus vaccine in cases of traumatic wounds[14] :
The authors point out that the severity of the wound should not be a factor in determining the need for tetanus immunization or prophylaxis.
Surgical management of open fractures involves adhering to a series of principles that have evolved over time and that are largely based on the care of war-wounded military personnel by military surgeons. A leading example is the work by Trueta, which described the successful use of debridement with splinting of injured extremities.[15] Introduction of invasive skeletal stabilization and continued focus on wound management led to increasing success. A modern protocol from Operation Enduring Freedom, by Lin et al, was not associated with any infections in 14 open fractures.[16]
It is critical to follow Advanced Trauma Life Support (ATLS) and institutional protocols to properly evaluate a trauma patient.[7] The preoperative evaluation must accurately document neurologic and vascular status. Digital photos are helpful for documenting the initial appearance of the extremity and can be a valuable addition to the medical record. Digital imaging allows other members of the treatment team to see the wound preoperatively without repeated manipulations of the wound.
Open fracture wounds can then be dressed with sterile, moist gauze, and clinical realignment of the limb can be accomplished with a temporary splint or traction. Patients who are appropriate for operative management should be urgently brought to the operating room.
Washing the wound with large volumes of fluid will remove macro contamination and clotting that may obscure the view of deeper levels of contamination or damaged tissue. Once the macro contamination is eliminated, the irrigation serves to diminish the residual bacterial contamination of the remaining healthy tissue. Irrigation is often done in conjunction with surgical debridement.
The use of antibiotics and other bactericidal additives to the irrigant continues to be a controversial treatment topic, but the chemical makeup of many of the additives is similar to that of soap and thus potentially can cause tissue swelling and the creation of surface layers over the damaged tissue.[17]
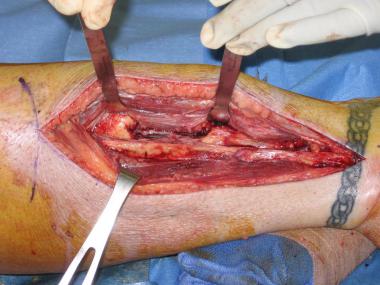
The debridement of an open fracture must be done in a thorough and systematic manner so as to avoid leaving devitalized tissue or contamination behind.[18] The skin edges of the traumatic wound should be trimmed to a healthy bleeding edge. Loose subcutaneous fat is also removed, along with any severely contused or noncontractile muscle. To ensure adequate debridement, traumatic wounds must be extended and muscle compartments opened and explored.
The removal of devitalized tissue is not limited to the soft tissues; bone should also be removed if it is free of soft-tissue attachment. Major articular fragments may be an exception to this rule; they should be retained whenever possible to allow for attempts at fixation and restoration of joint stability and motion. In general, the goal is to remove damaged tissue that would serve as a breeding ground for bacteria, without creating extensive additional surgical trauma by unnecessary periosteal stripping or undermining of the skin flaps.
In high-energy cases, it is often necessary to perform multiple debridements so as to adequately remove tissue that may evolve after the time of the initial operative inspection. In principle, it is best to avoid infection by removing devitalized bone and muscle and then to deal with later reconstruction by using bone grafting and soft-tissue flaps in an aseptic environment.
Fracture stabilization is critical for management of the injured extremity and for the overall benefit of the patient. The stability imparted to the bone helps minimize ongoing trauma to the soft tissues and provides a stable scaffold for tissue healing. Furthermore, bone stability allows for early functional motion of the extremity. Nursing care and mobilizing the patient out of bed are facilitated as well.
The choice of fracture-fixation method is based on many factors, including quality of local soft tissues, location and pattern of the fracture, overall health of the patient, and associated injuries. A detailed discussion of all the possible fixation methods for the variety of open fractures is beyond the scope of this article. Generally speaking, the method of fixation must minimize additional surgical trauma to the zone of injury while providing adequate stability for patient mobilization and soft tissue healing.
Some open fractures may benefit from the addition of local antibiotics. Antibiotics placed in the zone of injury can achieve high local concentration of the drug, typically without systemic side effects.[19] The technique involves antibiotic-impregnated beads sealed into the wound for gradual elution of drug to the surrounding tissues. The technique is based on the addition of heat-stable antibiotic powder to a batch of polymethylmethacrylate (PMMA) cement, forming beads that are threaded on nonabsorbable suture or wire.
The use of multiple small beads creates a relatively large overall surface area for antibiotic elution. Antibiotic cement spacers may also be used to preserve soft-tissue space in the presence of a significant bone defect; during a subsequent procedure, the cement spacer can be removed and the void filled with bone graft. An interesting aspect of this technique is that it has been shown that the pseudocapsule that forms around the cement has some osteogenic properties beneficial for promoting successful union after subsequent procedures.[20]
Commercially available preformed antibiotic beads are available and are typically made with a calcium-based, absorbable bead. These beads need not be removed at a subsequent procedure, and studies in animal models of contaminated open fractures using these systems appear to demonstrate promising outcomes.[21]
Although the practice has come under scrutiny, the prevailing method for dealing with open fracture wounds has been to perform serial debridements and close wounds in a staged fashion, particularly with type III injuries. Delayed wound closure became the standard on the basis of the experience of military surgeons and the severe consequences faced in dealing with primarily or prematurely closed wounds.
A common practice is to close the surgically created extensions of the traumatic wounds at the time of fixation and initial debridement, followed by a second look at the wound, with further debridement if necessary, in 48-72 hours. This can be repeated as indicated by the presence of any further evolution of tissue necrosis.
Vacuum-assisted closure (VAC) has become a popular technique for dealing with open fracture wounds. Some studies have suggested that the use of negative-pressure wound therapy (NPWT) may decrease the need for free tissue transfer or rotational flap coverage in high-energy open fractures. In many cases, abundant granulation tissue forms and residual soft-tissue defects can be covered effectively with basic skin grafts.[22, 23] (See the images below.)
 An open tibia fracture with bone loss. A tibial nail was placed and the wound was managed with negative pressure wound therapy, eventually covered with split-thickness skin graft.
An open tibia fracture with bone loss. A tibial nail was placed and the wound was managed with negative pressure wound therapy, eventually covered with split-thickness skin graft.
 Eight weeks later, the defect was approached from a lateral incision to avoid the previous medial open fracture wound. A central bone grafting technique was performed.
Eight weeks later, the defect was approached from a lateral incision to avoid the previous medial open fracture wound. A central bone grafting technique was performed.
 The central aspect of the leg was filled with bone graft, and internal fixation of the fibula was performed.
The central aspect of the leg was filled with bone graft, and internal fixation of the fibula was performed.
 The appearance of the mature synostosis 8 months after the patient's original injury.
The appearance of the mature synostosis 8 months after the patient's original injury.
Infection is the most obvious complication from open fracture.[5, 6] The risk of infection is related to the severity of the injury (see Classification of Open Fractures above), as follows[13] :
Failure to heal may result with any fracture. For of a variety of reasons, nonunion risk is greater with open fractures than with similar closed fractures. Many of the factors are related to the damaged blood supply at the zone of injury. The impaired circulation can lead to poor formation or loss of the fracture hematoma. The subsequent poor delivery of inflammatory mediators to facilitate callus formation and the presence of necrotic bone exacerbates the risk of nonunion.
Bone and/or periosteum loss from the fracture site impairs bone healing as well. Operative technique of debridement and fixation must focus on minimizing further trauma to the bone and surrounding tissues.
Details regarding outcome and prognosis for open fractures are variable, based on the specifics of the local and associated injuries.
The duration of postoperative antibiotic use is not clearly supported by the literature, but a common clinical practice is to continue perioperative antibiotics for 24-48 hours after each operative intervention until complete wound coverage or closure. Some of the literature strongly questions this practice, and concern has been raised regarding the development of resistant systemic nosocomial infections in the polytrauma patient because of overuse of perioperative antibiotics.[24] A modern study in the setting of current trauma care, fixation techniques, and antibiotic-resistance patterns is needed to clarify this issue.
In situations involving significant bone loss, the postoperative plan may include the use of autologous bone graft. In high-energy open fractures, the timing of subsequent grafting procedures should be based on the presence of a “fully reepithelialized wound with no drainage” and no clinical evidence of infection.[25]
The frequency of follow-up is driven by various factors. The wound may need to be monitored closely in the early phases of healing. The particular fractures and chosen methods of fixation will determine the need for radiographic and clinical reexamination. (See the images below.)
 An open midfoot fracture with bone loss at the base of the first metatarsal, including approximately 66% of the joint surface.
An open midfoot fracture with bone loss at the base of the first metatarsal, including approximately 66% of the joint surface.
 The foot was cared for with serial debridement and temporary pinning of the midfoot to preserve alignment with minimal additional surgical trauma.
The foot was cared for with serial debridement and temporary pinning of the midfoot to preserve alignment with minimal additional surgical trauma.
 An antibiotic-impregnated cement spacer was placed in the bone void, and 12 weeks later, after the pins had already been removed, a midfoot fusion was performed.
An antibiotic-impregnated cement spacer was placed in the bone void, and 12 weeks later, after the pins had already been removed, a midfoot fusion was performed.
 Intraoperative image of the midfoot fusion. The cement spacer has been replaced by autologous bone graft from the iliac crest.
Intraoperative image of the midfoot fusion. The cement spacer has been replaced by autologous bone graft from the iliac crest.
The principles for preoperative and intraoperative management of open fractures in the pediatric population are similar to those for adults, but there are a few differences that are largely related to the overall greater healing potential in this population.
In a review article, Stewart et al summarized each aspect of open fracture care for children.[26] They noted that initial evaluation and classification of the injury should follow the modified Gustilo-Anderson system, as in adults. The primary antibiotic choices are the same as in the adult population, but the authors cautioned against alternative regimens involving fluoroquinolones because of issues related to bone healing and chondropathy in children.
The timing of operative debridement has been studied retrospectively, and the results have called into question the dogma related to emergency management of open fractures in this population.[27] In one study, no difference in acute infection rate was found to be associated with operative care within 6 hours after injury as compared with operative care more than 7 hours after injury.
Further controversy stems from studies related to nonoperative management of type I open fractures, but the authors caution strongly against this practice without definitive study. Soft-tissue care generally follows that used in adults, and the use of vacuum-assisted closure (VAC) has been shown to be safe and effective in the pediatric population.[28] Fixation choices should account for the greater healing potential in children and, therefore, often do not require the same degree of stability as in adults.[26]
The timing of surgical intervention became controversial as a result of reevaluation of the literature upon which orthopedic dogma was founded—that is, that all open fractures must be operatively debrided and stabilized within 6 hours after the injury.
In 2006, Pollak authored a review of previous and more recent literature and concluded that "[the concept of] mandatory debridement within 6 hours of injury is minimally supported by the literature.”[29] Many studies that have utilized modern fixation strategies and immediate use of antibiotics have not shown a time-related difference in infection rate. As Pollak pointed out, a randomized trial in this area is not feasible, but additional study is needed to further illuminate the role that timing of initial surgical intervention plays on important outcome variables.[29]
Schenker et al published a systematic review and also concluded that the "6-hr rule" is not well supported by the existing literature. This was based upon the authors' close evaluation of 16 studies that included over 3500 open fractures.[30]
In clinical practice, it is likely to be in the patient’s interest to use a more practical, less dogmatic approach—namely, that open fractures should be treated surgically in an urgent (but not necessarily emergency) fashion, utilizing appropriate timely antibiotic coverage, skilled debridement, and skeletal stabilization.
The timing of wound closure is another area where the traditional dogma has been challenged. Again, the standard treatment is based on literature published before current standards related to antibiotics, surgical implants, and surgical technique. In short, it seems that, in many cases, primary wound closure at the time of operative debridement and fixation can be done safely without additional risk to the patient. As described by Weitz-Marshall and Bosse, “Surgical judgment, typically gained with experience, is required to successfully use an immediate wound-closure protocol."[31]
Weitz-Marshall and Bosse made the following additional suggestions[31] :
Very similar recommendations were made in a review paper published by Crowley et al[32] and include consideration of supporting literature published since the review described by Weitz-Marshall and Bosse.[31]
It is clear that irrigation is critical in the surgical management of open fractures, but the method of irrigation and the choice of irrigant solution are subjects of debate. An international survey of 984 surgeons described some of the differences in practice: 70.5% preferred normal saline, 16.8% added bacitracin, 6% added iodine-based solution, and 1.3% added a detergent or soap solution. Low-pressure modes of irrigation were preferred by 71%. The differences in practice reflect the variability in early and more recent studies.[33]
The conclusions of Crowley et al with respect to irrigation may be summarized as follows[32] :
A multicenter study by the FLOW investigators found that very low pressure (1-2 psi) was an acceptable, low-cost alternative for the irrigation of open fractures.[34]
Another area of both current controversy and future research pertains to the use of bone morphogenic protein (BMP). Although BMP may have many applications related to orthopedic fracture care, it has rarely been studied in relation to open fractures. A multicenter, prospective, randomized trial that studied the use of recombinant human BMP-2 (rhBMP-2) in open tibia fractures found that patients who received BMP at the time of their wound closure had lower infection rates and less frequent secondary intervention to obtain union.[35]
Certainly, cost is one controversial aspect of BMP therapy, but Jones et al showed that the use of BMP in open tibia fractures could result in a situation where the cost of the agent is offset, or even surpassed, by cost savings resulting from decreased secondary procedures and complications.[36] Further research is needed to define the proper patient and fracture populations in which BMPs are safe and effective adjuncts to open fracture care.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved