

Lumbar disc disease accounts for a large amount of lost productivity in the workforce. Accurate diagnosis can be difficult and often requires interpretation. Treatment is controversial. Surgical treatment can be technically simple and professionally gratifying for the surgeon. Treatment failures are not uncommon, are often related to posttraumatic or work-related injuries, and may result in litigation. As a consequence, this disease can generate distrust of physicians on the part of patients and vice versa.
This article clarifies some important guidelines for the diagnosis and treatment of lumbar disc disease.
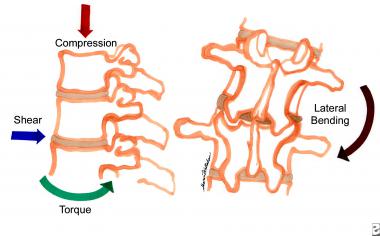 Degenerative lumbar disc disease. The various forces placed upon the discs of the lumbar spine that can result in degenerative changes.
Next
Degenerative lumbar disc disease. The various forces placed upon the discs of the lumbar spine that can result in degenerative changes.
Next
The first published report of lumbar disc herniation with radiculopathy was written by Mixter and Barr in 1934. Surgical treatment was not widespread until the 1950s. Today, lumbar discectomy is one of the most commonly performed elective operations in the United States.
Lumbar disc disease is a rather encompassing term. For example, some physicians include back pain alone as a symptom of disc disease. Others make the diagnosis without evidence of disc disease on MRI. The discussion of this article is limited to well-defined lumbar disc herniation. The pathophysiology, clinical presentation, radiographic diagnosis, treatment, and outcome are discussed.
Although most people experience back pain during their lifetime, only a fraction experience lumbar radiculopathy or sciatica as a consequence of root compression or irritation.
Almost 5% of males and 2.5% of females experience sciatica at some time in their lifetime.
A herniated disk fragment comes from the nucleus pulposus of the disc (a remnant of the embryonic notochord). In the normal condition, this nucleus is in the disk center securely contained by the annulus fibrosus.
When a fragment of nucleus herniates, it irritates and/or compresses the adjacent nerve root. This can cause the pain syndrome known as sciatica and, in severe cases, dysfunction of the nerve.
Most lumbar disc herniations (lumbar disc diseases) are preceded by bouts of varying degrees and duration of back pain. In many cases, an inciting event cannot be identified. Pain eventually may radiate into the leg. It may be characterized as less achy, burning, or similar to an electrical shock and is often described as a shooting or stabbing pain. The distribution of the leg pain is somewhat dependent on the level of nerve root irritation. Higher herniations (third or fourth lumbar levels) can radiate into the groin or anterior thigh. Lower radiculopathies (first sacral level) cause pain in the calf and bottom of the foot.
Fifth lumbar radiculopathy, which occurs most commonly, causes lateral and anterior thigh and leg pain. Often, accompanying numbness or tingling occurs with a distribution similar to the pain. Accompanying muscle weakness may be unrecognized if the pain is incapacitating. The pain usually improves when the patient is in the supine position with the legs slightly elevated. Patients are more comfortable when changing positions. Short walks can bring relief. Long walks or extended sitting (especially driving) can aggravate the pain.
On examination, patients may be neurologically normal, may have a profound radiculopathy, or may even demonstrate a cauda equina syndrome. A positive straight-leg raising sign is almost always present. However, a crossed straight-leg raising sign may be even more predictive of a lumbar disc herniation (lumbar disc disease). The back may appear scoliotic. Gait is often abnormal. Muscle weakness may be revealed particularly when testing walking on heels and toes.
The indications for surgical treatment of symptomatic lumbar disc disease are not clearly delineated. Nevertheless, situations exist in which most spine surgeons would probably agree on operative intervention. These situations include the following:
Notably missing from this list is a patient presenting with a profound motor deficit of varying duration. In the absence of pain, whether such patients benefit from surgery is unclear. No consensus has been reached concerning how urgent surgery is for a patient who presents with a clinical picture of painful disk herniation. Unfortunately, the decision to operate emergently is often based on fear of legal repercussions rather than on scientific evidence of actual patient benefit.
A disc herniation (lumbar disc disease) most frequently irritates the displaced nerve root. One of the more difficult concepts for beginning medical students to grasp is the anatomic relationship of the fifth lumbar (L5) nerve root to the L4-5 disc herniation.
Equally important to understand is the concept of the far lateral or foraminal disc herniation in which the root above the disc herniation is irritated.
With very large herniations, the entire cauda equina can be compressed and functionally compromised. This causes saddle anesthesia and can cause urinary retention and incontinence.
Any claim of absolute contraindications for lumbar disc disease would invariably be challenged. Most spine surgeons adhere to some guidelines, including the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved