

The purpose of this chapter is to discuss pelvic osteotomy as a means of stabilizing the hip and preventing early osteoarthritis. The different general categories of pelvic osteotomies commonly performed in current pediatric orthopedic practice are summarized, their principles are discussed, their indications are reviewed, and some of their key technical points are briefly explained.
The development of the hip socket (acetabulum) during the growth period depends largely on the interstitial growth within the triradiate cartilage. However, the concavity of the acetabulum develops in response to the presence of the spherical femoral head within it. Thus, any abnormality in the position of the femoral head with respect to the acetabulum during the growth period can produce an abnormal acetabulum.[1, 2, 3]
This altered congruency of the acetabulum resulting from its maldevelopment is referred to as acetabular dysplasia. More often than not, the concentric reduction of the subluxated or dislocated hip achieved at an early age takes advantage of the inherent growth of the acetabulum to ultimately obtain a well-developed acetabulum and a congruent hip joint.[1]
Some dysplasias of the acetabulum may persist until adolescence. Although the true incidence of persistent or residual acetabular dysplasia is unknown, it is well established that persistent acetabular dysplasia can lead to early degenerative joint disease.[4, 5] Emphasis is therefore placed on early recognition and timely treatment of persistent acetabular dysplasia by means of an appropriately selected pelvic osteotomy before any irreversible cartilage damage occurs.[6]
Pelvic osteotomy is a powerful surgical tool for realigning the dysplastic acetabulum and providing a biomechanically sound hip joint with essentially normal bearing surfaces. The goal is to preserve the natural bone and obviate the need for hip joint arthroplasty at a young age. Each type of pelvic osteotomy has its place, and each has its own advantages, disadvantages, and potential complications.
Selection of the proper pelvic osteotomy is the critical step in treatment. It depends on various factors, such as maturity of the triradiate cartilage, underlying disease and precise pathoanatomy of the hip joint in a particular case. The results of pelvic osteotomy are generally good, with remarkably durable restoration of the hip joint—provided that sufficient attention is paid to the indications for and the technical details of each particular osteotomy.
Pelvic osteotomies, though still in an evolutionary phase, have had a tremendous impact. By introducing the periacetabular osteotomy (PAO) and the concept of femoroacetabular impingement, Ganz et al[7, 8, 9] greatly changed the thinking of many surgeons involved in treating adolescents and adults with hip joint pathology requiring surgical treatment. Technical advancements in imaging are also helping practitioners detect and treat the degenerative process at a much earlier stage.
NextFor the surgeon planning a pelvic osteotomy, the anatomy of the posterior pelvic ligaments (ie, the sacrotuberous and sacrospinous ligaments) and the blood supply of the acetabulum are the 2 most relevant anatomic considerations.[10]
The sacrotuberous ligament is long, flat, and triangular. It is superiorly attached to the posterior superior and posterior inferior iliac spines, the back and the side of the lower part of the sacrum and the coccyx. The fibers converge below to end on the ischial tuberosity. The ligament is in line with the long head of the biceps femoris and may be considered as being derived from there. The posterior surface of the ligament gives origin to the gluteus maximus.
The sacrospinous ligament, also triangular in form, is attached by its apex to the ischial spine. Its broader base arises from the side of the lower sacral and coccygeal segments. This ligament converts the greater sciatic notch into the greater sciatic foramen. With the sacrotuberous ligament, which crosses it dorsally, it likewise converts the lesser sciatic notch into the lesser sciatic foramen.
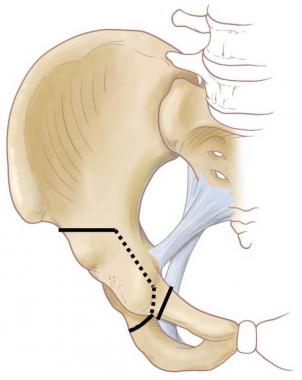
The attachment of these 2 ligaments in close proximity to the acetabulum has induced orthopedic surgeons to design a number of different ischial cuts (see the image below). The relevance of these ligaments during the performance of a pelvic osteotomy is addressed more fully elsewhere (see Redirectional Osteotomies).
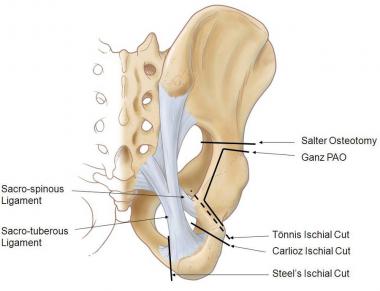 Posterior view of pelvis demonstrating lines of various pelvis osteotomies
Posterior view of pelvis demonstrating lines of various pelvis osteotomies
The acetabulum is supplied primarily by the periosteal arteries, with contributions from numerous local arteries. Each contributing bone carries its own vascular supply. The superior gluteal artery (SGA), the obturator artery (OA), and the superficial circumflex iliac artery (SCIA) contribute to the periosteal supply of the ilium. The pubis is supplied by a periosteal anastomosis of branches from the OA, the inferior epigastric artery (IEA), and the medial circumflex femoral artery (MCFA). The superficial and deep external pudendal arteries may also contribute.
Multiple vascular foramina are present, mainly at the lateral (acetabular) end of the bone, but there is no consistently placed nutrient foramen. The ischium carries multiple vascular foramina at its acetabular margin, along with a few on the pelvic surface. This bone is supplied by branches of the OA, the MCFA, and the inferior gluteal artery (IGA).
The risk of osteonecrosis of the acetabular fragment after periacetabular osteotomy (PAO) is one of the main arguments used by opponents of PAO.[11] However, a cadaveric study done by Beck et al using colored latex proved that even after PAO, the blood supply to the acetabulum is maintained through the OA and through the supra-acetabular and acetabular branches of the SGA.[12]
Similarly, a shelf acetabuloplasty or a Chiari osteotomy compromises the blood supply through the SGA, and the blood supply to the acetabular fragment will rely on the OA and on the branches of the MCFA to the anterior wall.[12]
In addition, surgeons should be acquainted with other normal musculoskeletal structures around the hip and some of the probable bony pathologic findings of the hip joint and pelvis in acetabular dysplasia. They should be comfortable with various surgical approaches to the hip and pelvis. Any combination of movement planes is possible within the limits of the restraining ligaments and muscular attachments.
In acetabular dysplasia, the stress across the hip joint is increased as a consequence of the following[13, 14] :
Accordingly, pelvic osteotomy is indicated to reduce the joint loading and increase the contact surface area; this undoubtedly affects cartilage and bone adaptation, resulting in beneficial joint remodeling.[13] Thus, pelvic osteotomy primarily redistributes the load (ie, changes the stress gradient) rather than changing overall hip joint pressure. Medialization of the hip joint center decreases the abductor muscles forces necessary to counteract the adductor forces and decreases the force across the hip joint.
The final goal of any pelvic osteotomy is to provide a stable hip joint, either by changing the shallow acetabulum into a deeper one or by redirecting the existing maldirected acetabulum and thus expanding the coverage of the femoral head by the native acetabulum. Besides normalizing the weight-bearing forces, pelvic osteotomies relax the capsule and muscles around the hip joint, improve the moment arm of the hip joint, and reduce the secondary stress on the lumbar spine by normalizing the anatomy and biomechanics of the whole pelvis.[13]
Because the pathomechanics of the hip joint vary greatly, depending on the age of the patient and the underlying pathology of acetabular dysplasia, and because there numerous different types of pelvic osteotomy, it is often difficult for a surgeon to predict which type of pelvic osteotomy will most improve the biomechanical environment in a given situation.
An abnormally shallow acetabulum can result from several developmental diseases of the hip joint. Invariably, acetabular dysplasia is a part of developmental dysplasia of the hip (DDH), which is the most common developmental hip disease. In addition, other childhood bony diseases, such as slipped capital femoral epiphysis and Legg-Calves-Perthes disease, can also produce residual acetabular dysplasia.
Acetabular dysplasia can also arise secondary to certain neuromuscular conditions, such as cerebral palsy (CP), Charcot-Marie-Tooth disease, myelomeningocele, and arthrogryposis.[15] It may be seen as an associated finding in syndromes such as Ehlers-Danlos syndrome and Larson syndrome. Essentially, any condition that interferes with the interdependent relation between the femoral head and the acetabulum during the growth period can lead to acetabular dysplasia.
The symptoms of acetabular dysplasia are directly related to its severity. Patients with mild acetabular dysplasia may remain pain-free until the fourth or fifth decade of life, or they may experience only vague discomfort with strenuous weight-bearing activities, particularly during the most productive years of their life. In the mild forms of pain-free acetabular dysplasia, abductor lurch or a limp is the only presenting symptom. Patients with severe acetabular dysplasia begin to experience pain in the second decade of life.
The patient’s activity level, functional status, and expectations are also contributing factors in the genesis of the symptoms. For instance, a severely dysplastic acetabulum in a nonambulatory cerebral palsy (CP) patient may be asymptomatic, whereas mild dysplasia in an adolescent athlete may be painful and may limit the activity level significantly. Thus, characterization of the patient’s symptoms should be individualized and should be correlated with the pathology underlying the residual acetabular dysplasia.
Lateral abductor-fatigue pain should be differentiated from anterior groin pain that is intra-articular in origin and indicates joint overload, with possible labral pathology or cartilage damage; the onset of degenerative changes is expected in such cases.
In deciding whether to reduce the hips, a distinction should be made between a patient who presents later with a unilateral dislocation and one who presents with bilateral hip dislocations. There are differences in the long-term health of the hip: bilateral dislocated hips tend to have better function without symptoms into adulthood, whereas a unilateral dislocation is more likely to have significant disability. In general, reduction of a unilateral hip dislocation is recommended up to 6-8 years of age; bilateral dislocations are more likely to be left alone at that age.
Physical examination starts with assessment of the patient’s gait. Any obvious limp or abductor lurch should be documented. A positive Trendelenburg test result (ie, dropping of the opposite pelvis with single-limb stance) indicates relative incompetence of the abductor mechanism, either from disuse atrophy secondary to pain or from a laterally displaced hip joint center requiring greater hip abductor muscle function. Extremities should also be carefully examined for muscle wasting and limb-length discrepancy.
Any abnormal limitation of rotational, sagittal plane, or coronal plane motions should be documented appropriately. Joint contracture, lower lumbar spine status, and pelvic obliquity should be assessed carefully. Significant pain with active or passive range of motion of the limb reflects synovitis or cartilage injury and should be documented correctly. The impingement test should be performed by means of hip flexion followed by adduction and internal rotation to assess the abnormal femoral head neck offset or labral damage.[16]
Further radiographic confirmation of the underlying cause of a positive anterior impingement test result can be obtained through magnetic resonance arthrography. This documentation is essential for finalizing the treatment protocol, in that a positive impingement test result is highly sensitive for diagnosing labral pathology that may be due either to overload that is secondary to a deficient anterior wall or to impingement that is the precursor of osteoarthritis.[14, 17]
All newborns should have a clinical examination for hip instability. Beyond that, however, newborn screening is controversial, with a spectrum of diagnostic tests available.
In North America, it is more common to rely on the initial history and physical examination and to refer for orthopedic evaluation and ultrasonography indicated only in the presence of a significant risk factor (eg, a first-born female with a breech presentation) or a significant physical examination abnormality (eg, a positive Barlow, Ortolani, or Galeazzi test result). The American Academy of Pediatrics has issued a practice guideline that generally follows these recommendations.
Others, especially in Europe, advocate ultrasonographic examination of every newborn to decrease the incidence of late dysplasia. The disadvantages of this approach include the substantial cost and the large number of infants with ultrasonographic abnormalities that then require treatment.
In the literature, the incidence of ultrasonographic abnormalities ranges from a low of 0.4%[18] to a high of 50%.[19] This wide range calls into question the utility of ultrasound screening of all newborns, especially when these radiographic abnormalities are associated with a normal physical examination, in which case nearly all of them resolve with time.[20]
Assessment of the acetabular anatomy via an appropriate radiographic view is the most essential preoperative step in the planning of any pelvic osteotomy. Radiographic evaluation starts with a plain anteroposterior (AP) radiograph of the pelvis with both hips in weight-bearing position (standing view), followed by frog-leg lateral and abduction-internal rotation (AIR) views of both hips and a false-profile view of the affected hip.
The AP standing radiograph is analyzed with respect to the intactness of Shenton’s line, the quality and the location of the acetabular sourcil, the acetabular index of the weight-bearing zone, the lateral center-edge angle of Wiberg, joint space narrowing, and the shape of the corresponding articular surfaces.
Shenton’s line is a continuous arc extending from the proximal medial femoral metaphysis onto the superior border of the obturator foramen. Any disruption in the continuity of this line indicates that the femoral head is proximally and laterally subluxated or dislocated.
The sourcil (French for “eyebrow”) is a dense layer of subchondral bone that normally appears as a smooth curve of uniform thickness and is a sensitive indicator of the location of loading of the hip joint. Any side-to-side asymmetry in the thickness of the sourcil indicates abnormal focal loading of the hip due to underlying acetabular dysplasia or joint malalignment.
The acetabular index of the weight-bearing zone[21] and the acetabular angle of Sharp[22] help quantitate the steepness of the acetabular wall (ie, the severity of the acetabular dysplasia).
The lateral center-edge angle of Wiberg[21] indicates the amount of femoral head covered by the acetabular roof.
Joint space narrowing is a rough guide to the loss of cartilage thickness on either of the articulating surfaces.
The AIR view neutralizes the femoral anteversion and simulates the coverage possible with either rotational pelvic osteotomy or proximal femoral varus osteotomy; it is essential for demonstrating a concentric reduction before the performance of a reorientation procedure.
The frog-leg lateral view gives a true lateral view of the proximal femur and helps assess any abnormal abutment of acetabular rim to the proximal femur in the flexed and externally rotated position of the limb. Quantitative assessment of head neck offset in this view is helpful for understanding the presence of any abnormal femoroacetabular impingement.
The false-profile view of Lequesne and de Sèze[23] is a true lateral view of the acetabulum made with the pelvis rotated 25° towards the x-ray beam. The anterior center edge angle measured on this false-profile view indicates the anterior extent of the acetabulum covering the femoral head.[23, 24]
Arthrography is a dynamic hip study that is performed by injecting contrast medium into the hip joint and then examining the hip directly under the image intensifier. The authors prefer a medial subadductor approach to injection of the dye. General anesthesia is usually required.
Arthrography is sometimes performed in the operating room immediately before the operation to provide a better understanding of the cartilaginous profile and a more accurate assessment of hip joint stability. The dynamic component of the test is sometimes useful for mimicking the coverage anticipated by the pelvic osteotomy.
Computed tomography (CT) with 3-dimensional reconstruction has contributed to a more precise understanding of the pathoanatomy of acetabular dysplasia. It gives the surgeon a 3-dimensional representation depicting the shape, orientation, and extent of the margins of the acetabulum, as well as the fit of the femoral head in the acetabulum. In this way, it can help the surgeon select the type of pelvic osteotomy that best matches the identified pelvic deficiencies.
Magnetic resonance imaging (MRI) and magnetic resonance arthrography are also indicated when associated labral pathology or cartilage damage is suspected. Magnetic resonance arthrography is the most sensitive indicator of the location and extent of a labral tear,[17] which can be clinically evidenced by anterior groin pain or a positive anterior impingement test result.[16]
Treatment is fundamentally surgical; little in the way of nonsurgical treatment can be offered. Symptomatic medical therapy, muscle-strengthening exercises, and weight-relieving exercises can be provided initially until the execution of the pelvic osteotomy. The goals are to eliminate hip irritability and instability and minimize the chances of further hip joint degeneration.
All pelvic osteotomies are planned to obtain an increased acetabular weight-bearing surface for the femoral head; this can be done either by redirecting or reshaping the acetabulum or by augmenting its margins. In general, pelvic osteotomies can be divided into 2 groups: reconstructive osteotomies and salvage osteotomies.
Reconstructive procedures are indicated in hips that have normal joint congruency with no cartilage damage and that reduce concentrically on an abduction-internal rotation (AIR) view. The aims of these procedures are to realign the joint surface and produce more normal loading and to delay or prevent the development of osteoarthritis. They have relatively predictable outcomes. Reconstructive osteotomies may be further divided into 2 subgroups: reshaping osteotomies and redirectional osteotomies.
Reshaping osteotomies change the shape and size of the acetabulum and are used only when the triradiate cartilage is open; they include the Pemberton and Dega osteotomies.
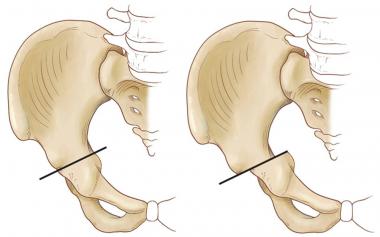
Redirectional osteotomies change the orientation of the acetabulum without changing the shape or dimensions of the acetabulum. These include the single innominate osteotomy of Salter; the double innominate osteotomies of Sutherland and Hopf; the triple innominate osteotomies of Steel, Carlioz, and Tönnis; and the periacetabular osteotomy (PAO) of Ganz (see the image below).
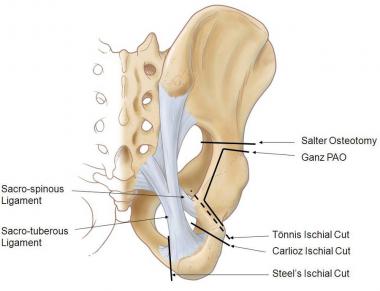 Posterior view of pelvis demonstrating lines of various pelvis osteotomies
Posterior view of pelvis demonstrating lines of various pelvis osteotomies
In contrast, salvage procedures are indicated for relieving pain, delaying the inevitable arthroplasty, and improving function in the meantime. They include the Chiari and shelf osteotomies. Salvage osteotomies are often performed on incongruent, already distorted hip joints. They often have less predictable outcomes than reconstructive osteotomies do.
Selection of a particular pelvic osteotomy depends on the severity of the acetabular dysplasia, the presence or absence of a congruent hip reduction, and the age of the patient. In a child aged 2-10 years who has a well-reduced hip with anterolateral acetabular deficiency of a moderate degree, either a Salter or a Pemberton procedure can be performed.
As an acetabular configuration-changing osteotomy, the Pemberton procedure in particular changes the shape and volume of the acetabulum and is primarily useful for a shallow, capacious, or wandering type of acetabulum[25, 26] .
The Salter osteotomy, on the other hand, is a redirectional procedure in which the innominate bone is transected completely and then rotated and tilted to provide anterior and lateral coverage of the femoral head without changing the true dimensions of the acetabulum. Thus, the Salter procedure is indicated in a young child with an acetabulum that is maldirected but has a normal configuration.[27, 28]
In an older child or adolescent with an open triradiate cartilage (usually over age 10), the triple innominate osteotomy is the procedure of choice. This procedure provides better mobility of the acetabulum and a wider range of coverage; however, it also necessitates more extensive dissection and more than 1 skin incision.
After the closure of the triradiate cartilage, PAO as described by Ganz[7] is the authors’ procedure of choice. This procedure gives extensive mobility to the acetabulum[7, 29] and affords the surgeon the opportunity to translate the hip joint center medially and thereby improve the biomechanical situation.[30] Moreover, PAO can be executed efficiently through a single skin incision.[31]
Patients with an incongruent hip joint are the most challenging for a surgeon to treat. If sufficient remodeling potential is present, a Salter or Pemberton innominate osteotomy may be considered. However, the outcome is always less predictable. Additional procedures (eg, a proximal femoral-shortening osteotomy) should also be considered, along with an acetabular procedure to decompress the joint, especially when an open reduction is required in patients older than 2-3 years.
In a patient older than 10 years, when almost no remodeling potential is left, a salvage procedure (eg, a shelf or Chiari osteotomy) is advisable. With the introduction of the Bernese PAO, many hips that were previously considered incongruent can be effectively treated, though treatment does involve considerable reorientation of the acetabulum and may require a proximal femoral osteotomy as well.[29, 32]
As the name implies, reshaping osteotomies are indicated to change the shape of a capacious or voluminous acetabulum, which is sometimes seen in developmental dysplasia of the hip (DDH) or cerebral palsy (CP) patients. Depending on the site of deficiency, the osteotomy is carried out to provide anterior or lateral coverage by levering the fragment down with the hinge over the triradiate cartilage. Thus, reshaping osteotomies are indicated in skeletally immature patients with an open triradiate cartilage.[33]
Because these procedures are incomplete osteotomies, additional fixation is usually not necessary, though external immobilization is often performed.
The Pemberton osteotomy is used for anteriorly and laterally deficient acetabula in patients older than 18 months who still have an open triradiate cartilage.[25, 26, 34, 35, 36]
A Smith-Peterson approach is used to access the inner and outer table of the iliac wing. The outer iliac cortex is osteotomized, with the cut started just above the anterior inferior iliac spine and carried out posteriorly and parallel to the capsule in the direction of the triradiate cartilage. The inner table is osteotomized if anterior coverage is necessary. Care must be taken to remain halfway between the anterior edge of the sciatic notch and the posterior rim of the acetabulum.
The osteotomy is opened sufficiently to bring down the anterior and lateral edges of the acetabulum. A rectangular graft is taken, beginning on the lateral aspect of the ilium and directed medially and posteriorly to avoid distorting the ilium. The graft is then reshaped to wedge between the distracted acetabulum to maintain correction, and a spica cast is applied for 6-8 weeks.
Reported complications include redislocation, sciatic nerve palsy, and femoral head osteonecrosis due to anterior pressure. Success is more predictable if the osteotomy is done in a patient younger than 4 years. Faciszewski et al reported a success rate of about 81% at 10 years after Pemberton osteotomy in a population of patients who were 4 years old at the time of surgery.[36]
The concept of the Dega osteotomy[37] is similar to that of the Pemberton osteotomy—that is, to change the configuration or shape of the capacious acetabulum by hinging the fragment through the open triradiate cartilage. However, unlike the Pemberton osteotomy, which increases anterolateral coverage, the Dega osteotomy involves cutting only the lateral aspect of the ilium and thus provides posterolateral coverage (see the image below).
 Dega Osteotomy
Dega Osteotomy
Posterolateral deficiency is often seen in the dysplastic acetabula of CP patients. The Dega pelvic osteotomy is a common procedure in this patient population and is often combined with a proximal femoral osteotomy.[38]
In redirectional osteotomies, the innominate bone is completely transected, and the acetabulum is shifted as a whole into a better position. Accordingly, such procedures are technically demanding and necessitate additional fixation or postoperative cast immobilization to maintain the new alignment until the osteotomy heals.
The Salter innominate osteotomy is indicated to correct a maldirected acetabulum in a child over 18 months of age, and is designed to cover the anterolaterally exposed femoral head.[39, 27, 28]
The principle is to redirect and rotate the existing acetabulum through the pubic symphysis and the sacroiliac joint in order to provide more anterolateral coverage of the femoral head. A concentric reduction of the femoral head in the true acetabulum in a skeletally immature patient (preferably younger than 6 years) is a prerequisite for the procedure. The young patient has a symphysis pubis pliable enough to allow rotation of the acetabulum to gain 20-22° of improvement in center-edge angle and about 10° of improvement in the acetabular index.
Given that the Salter osteotomy does not change the configuration of the acetabulum, a capacious acetabulum that requires volume reduction at the same time is a relative contraindication for this procedure.
Technical points
For optimal results, the femoral head should be able to reach below or to the level of the acetabulum preoperatively. Traction is recommended as needed to bring the femoral head down before the osteotomy.
Clearing of the sciatic notch before the iliac cut is a vital step. Traditionally, a Gigli saw is passed through the notch and directed anteriorly. The osteotomy should exit just above the anterior inferior iliac spine. However, the osteotomy can be performed by using a sharp osteotome from front to back, starting just proximal to the anterior inferior iliac spine.
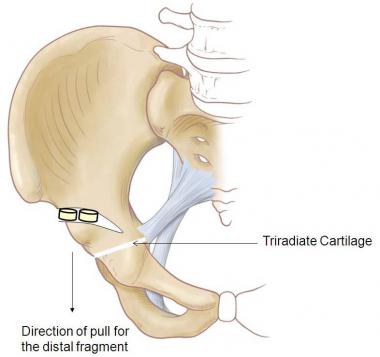
The distal fragment is then pulled caudally and anteriorly with a towel clip to obtain more anterolateral coverage (see the image below). Placing the ipsilateral foot on the opposite knee will provide a fair amount of flexion, abduction, and external rotation to relax the muscles of the affected hip and facilitate increased mobility of the acetabulum. An iliopsoas tenotomy is also warranted to help increase the mobility of the fragment, as well as to decrease the compression on the femoral head.
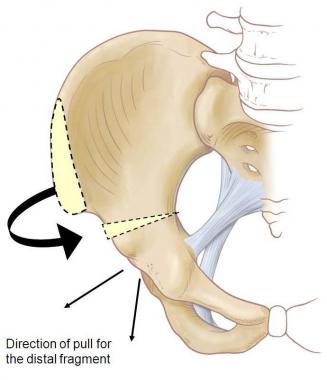 Salter Innominate Osteotomy: Distal fragment is pulled downward and forward
Salter Innominate Osteotomy: Distal fragment is pulled downward and forward
Care should be taken to prevent displacing the proximal fragment, which would lead to opening of the osteotomy posteriorly at the sciatic notch and lengthening of the affected limb. A triangular wedge-shaped graft, either from the anterior iliac crest or an allograft, is then inserted into the opening and fixed by 2 threaded pins or screws directed posteromedially. Hardware fixation not only prevents the loss of correction but also helps prevent graft collapse.
A single hip spica cast in 30-40° of flexion and abduction with slight internal rotation for 6 weeks is recommended postoperatively. The threaded pins can be removed in 6-8 weeks, depending on the radiographic union at the osteotomy site.
For a dislocated hip that is unstable at the time of reduction because of the steep slope of the acetabulum in a patient older than 18 months, a Salter innominate osteotomy is indicated along with an open reduction. If an open reduction is performed along with the osteotomy, a bilateral hip spica cast is preferred for 10 weeks.
Salter reported excellent to good long-term results in 93.6% of 140 patients younger than 4 years who were being treated for developmental dysplasia of the hip (DDH) but in only 56.7% of those older than 4 years.[39, 27, 28] Because of the unfavorable results with increasing age, the Salter innominate osteotomy is not advised for children older than 10 years.
Loss of correction, premature closure of the triradiate cartilage, redislocation or resubluxation, and sometimes even osteonecrosis of the femoral head due to increased joint pressure (especially when the osteotomy is done in association with open reduction) are the reported complications of the Salter innominate osteotomy.
Kalamchi suggested a modification of the Salter osteotomy that involved resecting a triangular wedge of bone from the posterior aspect of the proximal segment of the iliac bone without disturbing its far-end cortex, then fitting the posterior end of the distal fragment in that slot.[40]
This modification was intended to provide extra stability, decrease the displacement of the distal fragment, and decrease the intra-articular pressure. Furthermore, Kalamchi found this modification more useful in unilateral hip dysplasias where the ipsilateral limb is longer preoperatively.
An iliac crest bone graft is used to fill the triangular gap on the anterior aspect of the osteotomy, and 1 or 2 Steinmann pins are used to stabilize the osteotomy, much as in Salter’s description of the procedure. Postoperatively, a single hip spica cast in 25-30° of flexion and abduction with slight internal rotation is recommended for 6 weeks.
The single innominate osteotomy becomes more challenging after age 6-7 years because the stiffness of the symphysis pubis limits the mobility of the acetabulum. Consequently, in addition to the Salter osteotomy, some surgeons suggest dividing the pelvic bone to give the acetabulum increased freedom of rotation and to obtain the desired anterolateral coverage of the femoral head.
Double innominate osteotomy is often indicated in older children (often older than 6-7 years) or adolescents in whom more than 25° of coverage is desired. Concentric reduction of the hip joint with satisfactory cartilage space and congruity are the prerequisites for any type of double innominate osteotomy.
Double innominate osteotomy of Hopf
In the double innominate osteotomy of Hopf, the iliac osteotomy is similar to that in the Salter procedure. A second osteotomy is performed at the medial aspect of the acetabulum through the thin isthmus between the acetabulum and the pubis. The osteotomy is subsequently fixed with 1 or 2 Kirschner wires, and a hip spica cast is applied for 6 weeks. Reported complications include damage to the articular cartilage during the procedure and loss of position afterwards.
Double innominate osteotomy of Sutherland
In the double innominate osteotomy of Sutherland,[41] the first cut is similar to the Salter osteotomy, and the second cut is made just lateral to the symphysis pubis. The advantage of the Sutherland double innominate osteotomy is that it provides some medialization of the hip joint and minimizes the risk of injuring the growing triradiate cartilage in children and the articular cartilage in all age groups. However, an additional transverse suprapubic incision is needed, and this poses a degree of risk to the pudendal neurovascular structures.
Postoperative care and hip spica casting are similar to those recommended for the previously mentioned osteotomies.
In the initial report from 1977, Sutherland et al reported a 22° increase in center-edge angle and a 19.5° reduction in the acetabular index and recommended double innominate osteotomy in children older than 6 years.[41]
To further promote acetabular mobility in older children and those in whom greater correction is necessary, the triple innominate osteotomy was developed. In addition to the Salter osteotomy, osteotomies are made in the pubis and ischium to promote mobility and efficacious rotation of the acetabular fragment.
Because the complex anatomy of the ligaments of the hip capsule and the posterior area of the pelvis has generated controversy as to the best location for the pubic and ischial cuts, several different triple osteotomy procedures have been developed. However, a simple general rule may be formulated, as follows: The closer the osteotomies are to the hip joint, the greater the surgeon’s ability to rotate the acetabulum and obtain improved femoral head coverage.
Le Coeur was the first to describe a triple osteotomy of the pelvis. He advised cutting the superior and inferior pubic rami through a small incision on the medial aspect of the upper thigh. The ilium was transversely osteotomized through a Smith-Peterson approach just above the acetabular roof. The acetabulum was then rotated laterally and inferiorly to cover the femoral head.
Triple innominate osteotomy of Steel
Steel developed a surgical procedure in which the ischium is divided at the tuberosity through a posteroinferior approach with the patient supine.[42, 43] The ilium and pubis are then divided through an anterior approach similar to that used in the Salter osteotomy.
The disadvantage of the Steel osteotomy is that the ischial cut is below the sacrotuberous and sacrospinous ligaments, which means that these ligaments limit the mobility of the acetabulum. Steel’s triple osteotomy technique is therefore acceptable for mild to moderate acetabular dysplasia but not for hips in which a greater amount of acetabular reorientation is required.
The Steel osteotomy is recommended after closure of the ischial epiphysis. It is not suitable for hip dysplasia secondary to neuromuscular conditions such as cerebral palsy (CP), myelomeningocele, spina bifida, or Charcot-Marie-Tooth disease.[44] Other disadvantages of the Steel procedure include the following:
Lateralization of the hip joint has also been reported by some authors. Other complications associated with the procedure include paralytic ileus, myositis ossificans, nonunion of the ischium, and obstetric difficulties in female patients secondary to intrusion of the ischium.
Triple innominate osteotomy of Tönnis
Tönnis modified the triple innominate osteotomy by changing the location of the ischial cut.[45] The ischium is accessed through a posterior approach directly over the ischial tuberosity, and the ischial osteotomy is begun proximal to the sacrotuberous ligament and directed proximally so that it exits proximal to the sacrospinous ligament.
An advantage of the Tönnis osteotomy is the improved mobility of the acetabular fragment, which may be attributed to the bypass of the restraining ligaments, as well as to the close proximity of the osteotomy to the acetabulum.
Disadvantages include the technical complexity of the procedure and the close proximity of the ischial cut to the sciatic nerve (which is therefore at high risk). In a cadaveric study, de Kleuver et al determined that the femoral vein was also at risk during the pubic cut.[46] He further reported, on the basis of radiostereometric analysis, that 4 of 6 femoral heads were lateralized postoperatively.
As in most triple osteotomies the stability of the acetabular fragment is somewhat limited; consequently, a postoperative hip spica cast may be needed.
Triple innominate osteotomy of Carlioz
Carlioz developed a surgical technique in which the ischial osteotomy differs slightly from those of Tönnis and Steel.[47] In this variant, the ischial cut starts just below the acetabulum and runs horizontally in between the sacrospinous and sacrotuberous ligaments.
All 3 triple innominate osteotomies require a separate skin incision posteriorly over the ischial tuberosity. Anterior placement and fixation of the bone graft are essentially similar to the equivalent steps in the Salter procedure. Use of a temporary Schanz screw helps mobilize the fragment easily. Care should also be taken to prevent any muscle intervention between the cuts so as to avoid future nonunion.
As a consequence of the greater mobility of the distal fragment, a 33° improvement in the center-edge angle and approximately a 15° decrease in the acetabular angle of Sharp have been reported. Faciszewski et al reported a 94% success rate at 7 years.
In 1988, Ganz introduced the concept of periacetabular osteotomy (PAO) as a way of reorienting a dysplastic acetabulum after the closure of the triradiate cartilage. The aim of the procedure was to osteotomize the 3 pelvic bones close to the acetabulum so as to obtain maximal freedom of rotation and tilt of the acetabular fragment in the desired position in adolescents and young adults.[7]
The increased mobility of the acetabular fragment allows the surgeon to reorient the acetabulum in the sagittal and coronal planes while medializing the hip joint center, thus improving the biomechanics of the hip joint.[30] Other advantages of the Ganz PAO include the following:
Since the initial technical description of the procedure, an abductor-sparing approach has been developed in an effort to maintain the competence of this muscle group and thereby improve postoperative functioning. However, the learning curve of the Ganz PAO is steep.[50, 51] Major complications that have been reported in the literature include the following:
Reported minor complications include the following:
In a cadaveric study comparing the amount of motion of the acetabular fragment obtained with 3 different surgical techniques—Ganz, Tönnis, and Carlioz osteotomies—Aminian et al concluded that Ganz PAO provides maximum rotation and tilt of the acetabulum.[47]
In the authors’ opinion, the Ganz PAO has distinct advantages over any other type of triple innominate osteotomy, and their preference is to do the Ganz PAO as soon as the triradiate cartilage is closed. In an older child or adolescent in whom the triradiate is still open, the authors’ first approach is to delay the osteotomy in the asymptomatic patient until closure of the triradiate occurs. However, in symptomatic patients with an open triradiate cartilage, the authors prefer the Tönnis triple osteotomy.
Technical points
Via a single anterior skin incision and a modified Smith-Peterson approach, 4 cuts are made to release the acetabulum completely from the pelvis (see the image below).
 Anterior view of pelvis demonstrating lines of Ganz Periacetabular Osteotomy
Anterior view of pelvis demonstrating lines of Ganz Periacetabular Osteotomy
The first cut is made distal to the acetabulum and travels posteriorly toward the ischial spine; this cut requires the use of a curved Ganz osteotome. True anteroposterior (AP) and false-profile views using fluoroscopy are essential while the cuts are advanced.
The second cut is made in the superior ramus just medial to the iliopectineal eminence. It should be more oblique to assist in translating the joint medially.
The third cut (the supra-acetabular cut) is begun just distal to the anterior superior iliac spine. Only a small lateral window, made by stripping the abductor musculature, is necessary to execute this cut. This abductor-sparing approach helps in 3 ways: it keeps the blood supply of the acetabulum intact, it minimizes the formation of HO, and it assists in maintaining strong abductor function and avoiding a Trendelenburg lurch.
The fourth and final cut is made down the posterior column of the pelvis. This is done under fluoroscopic guidance with a false-profile view, allowing the surgeon to make the cut between the posterior margin of the acetabulum and the posterior aspect of the posterior column.
Once the osteotomies are complete, a Schanz screw is placed superior to the acetabulum and used to position the acetabular fragment; it is then fixed with provisional pins. Final optimal lateral and anterior coverage should be verified under imaging guidance while the normal version of the acetabulum is maintained.
Care should be exercised to avoid excessive anterior coverage, which can produce impingement leading to labral and cartilage damage. After the positioning of the acetabular fragment, the hip should be flexed to 90° to ensure that impingement has not been created.
Definitive fixation is achieved with 3 or 4 threaded cortical screws (either 3.5 mm, as the authors prefer, or 4.5 mm) placed fully through the iliac wing, in addition to a screw from the superior aspect of the acetabular fragment to the ilium.
Salvage osteotomy is indicated for an incongruently reduced hip joint or a painful joint in which the remaining cartilage is not sufficient to allow it to be brought over the weight-bearing position by any of the previously mentioned redirectional or reshaping osteotomies. Salvage procedures may be appropriate for an adolescent or adult patient with a painful, subluxated hip or for a patient with previous surgical failure.
Salvage osteotomies mainly rely on the metaplasia of the capsule to provide an extension of the articulating surface. The authors rarely use such procedures in young adolescent patients, because the versatility of the Bernese periacetabular osteotomy (PAO) makes it possible to achieve outstanding correction and effectively treat even the worst dysplastic situation.
The Chiari osteotomy relies on a laterally displaced ilium that supports the femoral head with interposed capsule as an interposition-style graft; the assumption is that fibrocartilage develops between the femoral head and the ilium.[54, 55, 56, 57] The procedure brings the hip joint medially, in addition to expanding the contact area of the femoral head. Femoral head coverage is dependent on the width of the ilium.
Technical points
Via an anterolateral approach, the inner and outer tables of the iliac wing are exposed to the sciatic notch. The ilium is osteotomized between the capsule and the reflected head of the rectus. The osteotomy follows the capsular insertion in a curved line to the sciatic notch posteriorly and the inferior iliac spine anteriorly. The acetabulum is displaced medially by forced abduction with rotation through the pubic symphysis, so that the femoral head is covered without the fragments being completely separated (see the image below).
 Chiari Osteotomy
Chiari Osteotomy
Traditionally, the osteotomy is fixed with threaded pins, supplemented with a hip spica cast for approximately 6 weeks. An additional shelf procedure is sometimes needed to provide adequate coverage.
Windhager et al reported long-term good to excellent results in 52% of patients. However, results worsen with increasing patient age and higher degrees of joint degeneration present before surgery. Incomplete medialization and limited range of motion are the reported complications of Chiari osteotomy.
Shelf osteotomy (shelf acetabuloplasty) provides an extra articular buttress to prevent the subluxation of the femoral head and to expand the load-bearing area of the hip joint.[58, 59, 60, 61, 62, 63, 64, 65] A shelf osteotomy is also indicated when augmentation of the acetabulum is needed even after another pelvic osteotomy has already been done.
Various surgical measures have been described to provide better coverage, such as reflection of the outer cortex of the iliac wing down over the capsule, use of the slotted shelf procedure, and intracapsular incorporation of the shelf.
Technical points
Via a Smith-Peterson approach, the reflected head of the rectus is sharply divided. A 1-cm-deep slot is created just above the capsule, extending anteriorly and posteriorly according to the amount of coverage desired and the contour of the capsule. A corticocancellous graft is firmly inserted into the slot and is secured to the underlying capsule with 2 holding sutures.
The lateral wall of the ilium just above the graft is roughened with a burr, and the corticocancellous graft is kept over the shelf to enhance the rate of union. The reflected head of the rectus is tied back to secure the graft and to hold the shelf with the downward-slanted lateral edge of the graft.
After completion of the shelf, the range of motion of the hip joint should be checked carefully to confirm that there is no impingement by either the femoral neck or the greater trochanter.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved