

Genu varum is a Latin term used to describe bow legs. This condition may present from infancy through adulthood and has a wide variety of causes. As it becomes more severe, the patient may exhibit lateral knee thrust and a waddling gait. There may be associated in-toeing and secondary effects on the hip and ankle. The problem may be unilateral, with a functional limb-length discrepancy, or bilateral. The family and medical history may reveal clues to the likelihood of persistence or progression.
It is widely recognized that up to age 2 years, infants may have physiologic bowing of the lower extremities. The hallmark of this condition is symmetrical and painless bowing, usually associated with in-toeing and often with a propensity for tripping. This problem will resolve spontaneously without treatment, as a result of normal growth.[1, 2, 3] All that is required is parental education and periodic follow-up to verify resolution. During the wait for the predicted spontaneous correction, reversing the shoes may reduce the frequency of tripping.
The prevalence of this condition is not known, but it is frequent enough to be considered a variation of normal in toddlers. Nevertheless, it is a relatively common cause of parents’ seeking medical attention from their primary care providers, who should be knowledgeable in the triage of these conditions. Only in the most persistent or worrisome cases is orthopedic consultation warranted. Radiographs, though optional as a rule, may be needed to differentiate physiologic varus from pathologic conditions that call for treatment.[4]
NextIn normal alignment, the lower-extremity lengths are equal, and the mechanical axis (center of gravity) bisects the knee when the patient is standing erect with the patellae facing forward (see the image below). This position places relatively balanced forces on the medial and lateral compartments of the knee and on the collateral ligaments, while the patella remains stable and centered in the femoral sulcus.
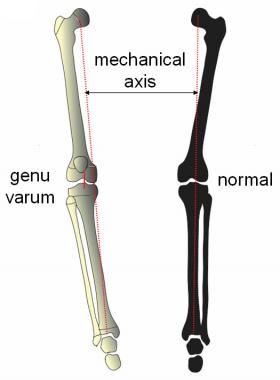 Mechanical axis is measured on full-length weightbearing radiograph by drawing line from center of femoral head to center of ankle. Normally, it should bisect knee, with joint horizontal and parallel to ground. Genu varum is defined by medial displacement of mechanical axis. Shown here is varus of tibia and slight lateral ligamentous laxity contributing deformity.
Mechanical axis is measured on full-length weightbearing radiograph by drawing line from center of femoral head to center of ankle. Normally, it should bisect knee, with joint horizontal and parallel to ground. Genu varum is defined by medial displacement of mechanical axis. Shown here is varus of tibia and slight lateral ligamentous laxity contributing deformity.
In children younger than 2 years, physiologic genu varum is common but is self-limiting and innocuous. In older children with pathologic varus, as the knee drifts laterally, the mechanical axis falls in the inner quadrant of the knee; in severe cases, it does not even cross the knee (see the image below).
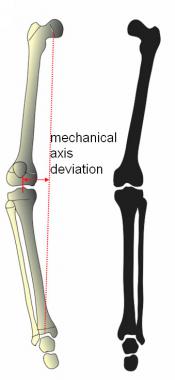 Three factors contributing to genu varum: varus femur, ligamentous laxity, and varus tibia. Mechanical axis is further deviated medially.
Three factors contributing to genu varum: varus femur, ligamentous laxity, and varus tibia. Mechanical axis is further deviated medially.
As a result, the medial femoral condyle and the medial plateau of the tibia are subjected to pathologic loading. The Heuter-Volkmann effect will compress the physis and the cartilaginous anlage of these structures and inhibit the normal ossification of the epiphysis. The lateral collateral ligaments are stretched, sometimes beyond their compliance, permitting the characteristic lateral thrust of the knees during gait.
When the mechanical axis deviates into or beyond the medial quadrant of the knee, regardless of the etiology, a number of clinical problems may ensue. Lateral ligamentous strain may be associated with recurrent knee pain, lateral thrust, in toeing, and the evolution of a waddling gait.
The natural history of untreated genu varum is not benign. During the adult years, premature and eccentric stress on the knee may result in medial meniscal tears, tibiofemoral subluxation, articular cartilage attrition, and arthrosis of the medial compartment of the knee. Nonoperative management that relies on shoe modification, physical therapy, and so-called Forrest Gump bracing is of no proven value.
The recognized etiologies for genu varum include the following:
 Tibia vara (Blount disease) is growth disturbance of proximal medial tibia that can present any time from infancy to adolescence. Natural history is one of inexorable progression, premature closure of upper medial tibial physis, lateral thrust, ligamentous laxity, and, ultimately, joint instability and degeneration. At age 5, guided growth would have been sufficient. After physeal closure, complex osteotomies are required.
Tibia vara (Blount disease) is growth disturbance of proximal medial tibia that can present any time from infancy to adolescence. Natural history is one of inexorable progression, premature closure of upper medial tibial physis, lateral thrust, ligamentous laxity, and, ultimately, joint instability and degeneration. At age 5, guided growth would have been sufficient. After physeal closure, complex osteotomies are required.
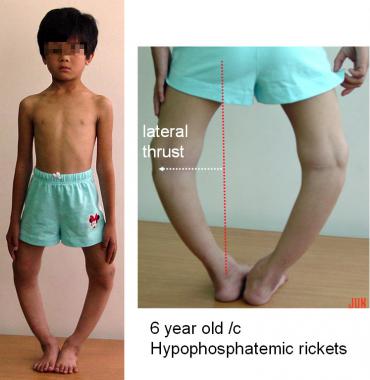 Hypophosphatemic rickets is disturbance in vitamin D metabolism that weakens physes through delayed ossification. Consequent deformities may progress despite careful medical management and bracing. Deformities are typically bilateral, involving both femur and tibia.
Hypophosphatemic rickets is disturbance in vitamin D metabolism that weakens physes through delayed ossification. Consequent deformities may progress despite careful medical management and bracing. Deformities are typically bilateral, involving both femur and tibia.
Regardless of the etiology of pathologic genu varum and regardless of the patient’s age, surgical correction of significant and symptomatic malalignment is warranted.
Physiologic genu varum, defined as occurring in children younger than 2 years, is exceedingly common but is self-correcting. In contrast, pathologic genu varum, which is due to a variety of conditions, is much less prevalent, especially with increasing age. Among the known causes are tibia vara (Blount disease), rickets, and skeletal dysplasias. The collective frequency of these conditions is not specifically known, but they are common triggers for pediatric orthopedic referral.
In countries where malnutrition is widespread and access to medical care is limited, the overall incidence of genu varum is undoubtedly higher. Whereas polio has been largely eradicated, other infectious diseases and mistreated (or untreated) traumatic injuries make physeal damage a frequent cause of progressive and disabling clinical deformity.
Likewise, untreated congenital anomalies, genetic disorders, metabolic conditions, and rheumatologic diseases may all cause progressive genu varum. Finally, in any country, one may encounter iatrogenic postoperative genu varum.
The outcome of guided growth for genu varum is dependent on patient selection and timing. As noted earlier, this technique is contraindicated for physiologic genu varum and will be of no benefit after skeletal maturity has been attained. At least 6 (and preferably 12) months of predicted growth is needed to derive any benefit.
For the remainder of patients, regardless of age or diagnosis, guided growth holds promise for complete correction of the deformity and may reduce or eliminate the need for more invasive osteotomies. For specific endocrinologic conditions, concomitant medical management is required.
The parents must have a vested interest in the success of the procedure and must understand that although the incisions are small and the correction gradual, the onus is on them to return for follow-up appointments at the specified intervals (typically every 3 months while the implants are in place).
It is most helpful to ask the child with genu varum to stand with feet together and with equal weight on both legs. The intercondylar distance is easy to measure and demonstrate to the concerned parents. Observe the gait noting the foot progression angle and the presence or absence of a lateral thrust. In the prone position, measure the inward-outward hip rotation (femoral torsion) and the thigh-foot axis (tibial torsion).
In addition, examine the entire spine and record the stature of the child. Document the range of hip motion, including abduction in flexion and extension. Children with dysplasias or metabolic disorders may have coxa vara, limited hip abduction and a positive Trendelenburg gait. They may also have ankle varus with medial thigh and calf creases.
When an underlying syndrome is suggested by the physical findings and history, consultation with a geneticist and an appropriate workup are warranted. If metabolic bone problems are a concern, relevant hematologic and urine studies are warranted, along with consultation with an endocrinologist. In a select few patients, bone densitometry studies may be warranted.
Plain radiography is the only diagnostic procedure required in most cases. The gold standard of radiographic documentation is the full-length weightbearing anteroposterior (AP) view of the lower extremities, taken with the patellae facing forward. In addition to the knee deformities, there may be varus of the proximal femur or the distal tibia or fibula.
The relevant anatomy, in addition to possible hip and ankle deformities, includes the distal femoral and proximal tibial physes, either or both of which may contribute to varus malalignment. A simple screening test is to view the full-length AP radiograph with the knee in a horizontal plane. When the film is oriented so that the knee is on a horizontal plane, it may be readily apparent whether the femur, tibia, or both are contributing to the deformity and therefore which level or levels should be addressed.
The best way of measuring and determining which physes are contributing to deformity is to measure the anatomic joint-shaft angles at each level. These include the lateral distal femoral angle (LDFA), which is normally 84°, and the proximal medical tibial angle (PMTA), which is normally 87° (see the image below).
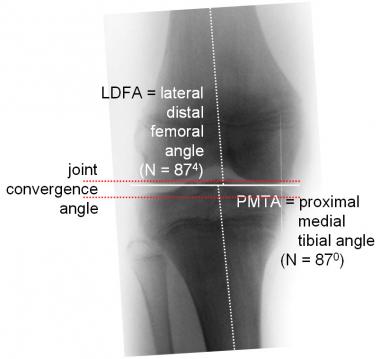 Anatomic angles are measured between joint surface of each bone and its respective shaft. Lateral distal femoral angle (LDFA) is normally 84°, and proximal medial tibial angle (MPTA) is 87°. On close-up view, one can measure joint convergence angle (normally 0°); this is defined by articular surface lines of femur and tibia. Lateral ligamentous laxity can contribute to varus malalignment.
Anatomic angles are measured between joint surface of each bone and its respective shaft. Lateral distal femoral angle (LDFA) is normally 84°, and proximal medial tibial angle (MPTA) is 87°. On close-up view, one can measure joint convergence angle (normally 0°); this is defined by articular surface lines of femur and tibia. Lateral ligamentous laxity can contribute to varus malalignment.
In addition, when the lateral ligaments are incompetent, measuring the joint convergence angle or obtaining a varus stress AP radiograph may demonstrate their respective contributions to the clinical deformity. It is important to remember that there may be sagittal-plane and rotational deformities that confound the analysis and treatment.
In contradistinction, scanograms are of questionable value because they are not weightbearing, do not demonstrate diaphyseal deformities, and do not show the mechanical axis.
Aside from a well-documented clinical examination and gait observation (repeated as necessary to document progression) and the standard radiographs already mentioned, other tests generally are not indicated. Unless a physeal bar is suspected (which is unusual), there is no need to resort to computed tomography (CT) or magnetic resonance imaging (MRI).
In select cases, gait analysis may be interesting, but it will not determine either the need for or the timing of intervention.
Depending upon the underlying etiology of genu varum, epiphyseal, physeal, or metaphyseal histologic abnormalities may be present, and bone density may be diminished. However, biopsy of the bone is rarely necessary or helpful. Such invasive procedures may have an adverse effect upon physeal growth and the outcome of treatment.[5]
For physiologic genu varum, parental reassurance is required, but no treatment is necessary; spontaneous resolution by the age of 2 years is the rule. In borderline cases, continued follow-up is warranted.
To resolve pathologic genu varum, some have relied on so-called Forrest Gump above-the-knee braces. However there are no controlled, randomized trials that support the efficacy of such treatment. Furthermore, the laxity of pediatric collateral ligaments may militate against such a management strategy because the force applied by the braces may be expended upon the ligaments. The cost and restrictive nature of such braces further diminish compliance.
In defined metabolic conditions, such as rickets, medical management is paramount for success. There may be other appropriate measures that should be taken, such as dietary management for celiac sprue, administration of bisphosphonates in select cases of osteopenia, and gene therapy for collagen storage disorders.
There are a variety of options for intervention, ranging from attempted bracing to osteotomy. Bracing was popular until the mid-1900s, but enthusiasm for this approach has now largely dissipated as a consequence of problems with brace design and cost, patient noncompliance, and unproven efficacy.
At the other end of the treatment spectrum is osteotomy, which involves cutting the femur, the tibia/fibula, or both, depending upon the level or levels of bony deformity.[6, 7] However, osteotomies are relatively invasive and fraught with potential complications (eg, failure of fixation, physeal damage, infection, joint stiffness, compartment syndrome, neurovascular injury, over- or undercorrection, and recurrent deformity).[8, 9] Some of these pathologic varus deformities are bilateral and multilevel, which increases the risk of problems.
Phemister was the first to operate directly on the physis for the purpose of correcting length discrepancy or changing angles.[10, 11] His technique involved removing and rotating a rectangle of bone spanning the physis so as to create a permanent bone bridge for tethering the physis.
Besides its relatively invasive nature, the main limitation of this procedure is that it is permanent. Whereas other techniques employed fluoroscopy to permit percutaneous drilling and minimize the impact and scars, the permanence of this method necessitates meticulous planning, accurate determination of bone age, and close follow-up to avoid overcorrection.[12, 13, 14]
Guided growth is a minimally invasive and modular method of correcting genu varum in the pediatric patient. The key advantage of this intervention is its temporary and reversible nature. The historical methods of mechanical restraint of a given physis began with Blount in 1949 and were promulgated by others for the latter half of the 20th century.[15, 16, 17, 18, 19, 20, 21]
However, problems experienced with staples, including migration or breakage and the necessity of premature revision surgery, detracted from the popularity of this approach and led to the development of alternative methods, including the percutaneous transphyseal screw[22] and, subsequently, the eight-Plate (Orthofix, Verona, Italy).[23, 11, 24] Alternatives to the eight-Plate that appear to have comparable efficacy but greater cost-effectiveness have been studied.[25, 26]
The natural history of untreated pathologic genu varum is one of inexorable progression and associated gait disturbance. The indications for surgical intervention are partly clinical, based on documented progression, and partly determined by radiographic criteria.
Once the child has achieved independent ambulation, early intervention may enable simpler treatment via guided growth. This method is applicable throughout the growing years and may be repeated as deemed necessary. After skeletal maturity has been reached, corrective osteotomies may be required to correct malalignment.
In advanced cases, both the femur and the tibia/fibula may have to be addressed, preferably before ligamentous laxity complicates matters. Concomitant varus of the proximal femur or the distal tibia/fibula may also warrant correction. The longer the surgeon waits to correct the knees, the more likely it is that these confounding variables will require attention.
There are only two contraindications for surgical correction of genu varum, as follows:
The era of rigid physeal constraint (with staples and screws) may be drawing to a close. The advantages of a flexible tension band are evident: more rapid correction and fewer hardware-related problems. However, plate retrieval is still necessary. Perhaps biodegradable implants will be available one day. The challenges related to the control and planned obsolescence of such implants still must be addressed. In the future, guided growth via chemical, thermal, or electrical manipulation or via targeted radiofrequency signaling may become a reality.
The requisite clinical examination should include measurement of the intercondylar distance, limb lengths, torsional profile, and gait observation; preoperative radiographic documentation that includes measurement of the mechanical axis deviation and the femoral and tibial joint-shaft angles is also essential (see Workup).
If there is doubt as to the etiology or natural history of genu varum, it is helpful to repeat the examination at 3- or 6-month intervals, with comparative radiographs as needed, before formulating a treatment plan. Bracing, though advocated by some, is expensive and unwieldy. More important, it may not have a proven beneficial effect on the natural history of a given deformity.
Beware of unilateral or asymmetrical deformities; it is hard to rationalize these away as instances of physiologic genu varum.
It is helpful to document medial displacement of the mechanical axis; progression of this displacement after the age of 2 years serves as a relative indication for surgical intervention. Generally speaking (except in the case of physiologic varus), when the mechanical axis is in medial zone 2, there is a relative indication for intervention, and when it is in zone 3, there is an absolute indication (see the image below).
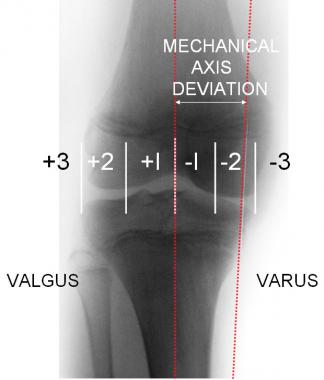 If knee is divided into quadrants and variations of normal allowed for, mechanical axis should be neutral or at least fall within medial or lateral zone 1. Deviation into zone 2 is relative indication for surgical intervention, and zone 3 is obvious call for action. If physes are open, correction may be gained by guided growth; after skeletal maturity, only choice is corrective osteotomy.
If knee is divided into quadrants and variations of normal allowed for, mechanical axis should be neutral or at least fall within medial or lateral zone 1. Deviation into zone 2 is relative indication for surgical intervention, and zone 3 is obvious call for action. If physes are open, correction may be gained by guided growth; after skeletal maturity, only choice is corrective osteotomy.
It may be deleterious to correct a pan-genu deformity at 1 level; doing so will induce an undesirable slope of the knee with late consequences. If there is concomitant varus of the proximal femur or distal tibia, these may have to be addressed as well. Inward torsion of the tibia may actually improve spontaneously after guided growth. Thus, it is safe to defer treatment of perceived torsional deformities pending angular correction. Later, one can always perform a supramalleolar rotational osteotomy, which is safer than a proximal osteotomy.
Guided growth (temporary hemiepiphysiodesis) may be the treatment of choice for most children with progressive genu varum, even those with “sick physes.” The lateral distal femoral or lateral proximal tibial physes may be temporarily restrained with an eight-Plate. This approach offers proven advantages over the Blount staples that were introduced in the 1940s: Plates are more secure than staples and will not dislodge, and screw breakage is exceedingly rare. This technique may be undertaken in children aged 18 months to 18 years, provided that the physes are open.
The goal of guided growth is to restore the mechanical axis to neutral, thus mitigating the cumulative effects of gravity on the overloaded structures, alleviating the pain and gait disturbance, and helping to protect the knee throughout the growing years. When a reversible technique such as placement of the eight-Plate is employed, the physis will continue to grow during guided growth, and this physeal growth will continue unabated after the implant is removed.[23, 11, 27]
The time to correction ranges from 6 to 24 months, but typically the mechanical axis is corrected within 12 months of insertion. In most cases, the proximal fibula need not be tampered with.
When the mechanical axis has been restored to neutral, the implants are removed. Subsequent growth should be monitored. Depending on the etiology, there may be recurrent deformity due to rebound growth; this is best managed by repeating the guided growth procedure. Even if repeated (albeit minor) intervention is required, the benefits still outweigh the cost and risks of (sometimes) repeated osteotomies. Consequently, osteotomies can be deferred for subsequent correction of persistent rotational or length issues as necessary.
The steps in the technique are as follows:
It is important to keep in mind that these titanium plates, by design, are nonlocking. Their strength is predicated on their ability to serve as a flexible tension band that can bend as the screws reach their maximum divergence (~30°). At maximum divergence, the flexible plate will gradually begin to reverse-bend, permitting further angular correction. Screw length is not highly critical, but screws should not be so long that they violate the far cortex.
Guided growth with the eight-Plate (see the images below) offers a high success rate, with few and minor complications.[28]
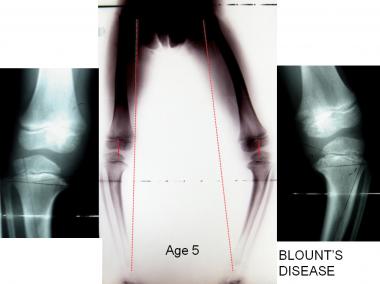 At age 5, this boy presented with asymmetrical tibia vara (Blount disease). Treating surgeon employed guided growth on right and osteotomy of tibia/fibula on left.
At age 5, this boy presented with asymmetrical tibia vara (Blount disease). Treating surgeon employed guided growth on right and osteotomy of tibia/fibula on left.
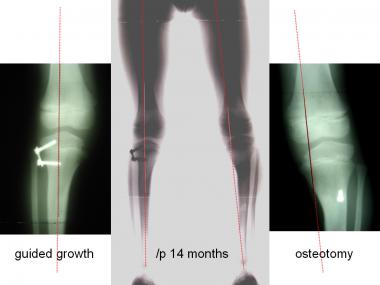 At 14-month follow-up, mechanical axis is neutral on right, and plate was removed. Mechanical axis was in medial zone 2; this was addressed by insertion of lateral eight-Plate.
At 14-month follow-up, mechanical axis is neutral on right, and plate was removed. Mechanical axis was in medial zone 2; this was addressed by insertion of lateral eight-Plate.
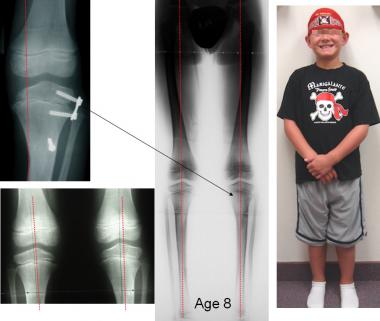 After additional 8 months of guided growth, leg straightened out, and plate was removed. Patient's limb lengths remain equal, and there has been no recurrence of angular deformity. Annual monitoring will continue until maturity: if there is any drift of mechanical axis, guided growth will be repeated.
After additional 8 months of guided growth, leg straightened out, and plate was removed. Patient's limb lengths remain equal, and there has been no recurrence of angular deformity. Annual monitoring will continue until maturity: if there is any drift of mechanical axis, guided growth will be repeated.
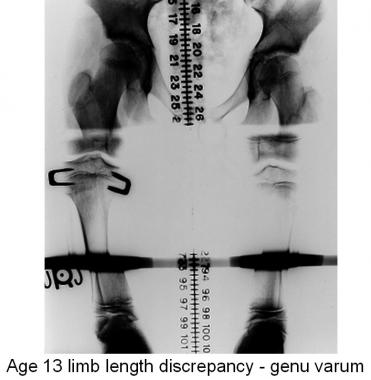 At 1 year after proximal tibial stapling to correct limb length inequality, this scanogram shows loosening of lateral staples with consequent iatrogenic varus of tibia. Physes are still open.
At 1 year after proximal tibial stapling to correct limb length inequality, this scanogram shows loosening of lateral staples with consequent iatrogenic varus of tibia. Physes are still open.
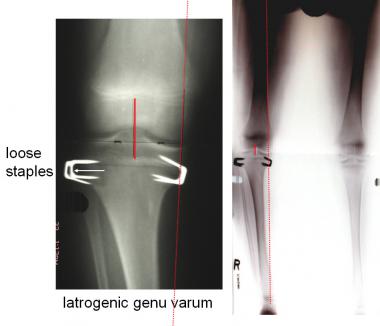 Full-length view shows mechanical axis deviation into medial zone 2; this was not demonstrable on scanogram. Staples were removed and lateral ones replaced with eight-Plate.
Full-length view shows mechanical axis deviation into medial zone 2; this was not demonstrable on scanogram. Staples were removed and lateral ones replaced with eight-Plate.
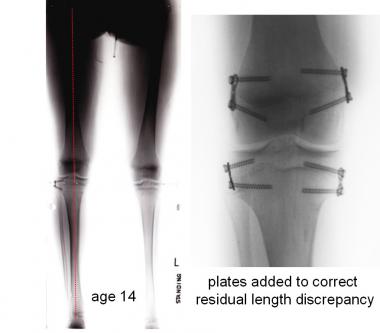 At 1 year after guided growth with eight-Plate, mechanical axis has been restored to neutral. At that time, eight-Plates were employed to accomplish pan-genu epiphysiodesis to correct patient's residual limb length inequality.
At 1 year after guided growth with eight-Plate, mechanical axis has been restored to neutral. At that time, eight-Plates were employed to accomplish pan-genu epiphysiodesis to correct patient's residual limb length inequality.
In situations that preclude guided growth (physeal closure or skeletal maturity) it may be necessary to cut the femur or the tibia and fibula to accomplish the desired realignment (see the images below). The goal of osteotomy is to realign the extremity and provide a neutral mechanical axis while correcting malrotation and restoring equal limb lengths. However, this procedure comes with significant associated risks and costs.[8, 9] Furthermore, if there is recurrent deformity, realignment becomes more difficult with each subsequent endeavor.
 This 7-year-old boy with Ollier disease presented with complex deformity including varus and outward torsional deformity of right tibia and progressive limb length discrepancy. Whereas guided growth could improve varus, it could not address other two issues. Therefore, he underwent osteotomy and callotasis with Taylor Spatial Frame.
This 7-year-old boy with Ollier disease presented with complex deformity including varus and outward torsional deformity of right tibia and progressive limb length discrepancy. Whereas guided growth could improve varus, it could not address other two issues. Therefore, he underwent osteotomy and callotasis with Taylor Spatial Frame.
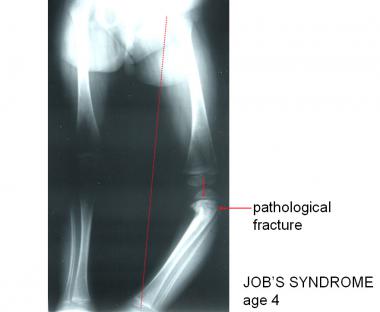 This 4-year-old girl with Job syndrome, which includes immunoglobulin deficiency, had osteopenia and developed pathologic fracture of proximal tibia. She then drifted into progressive genu varum. It was felt that guided growth might not work in mechanically compromised environment.
This 4-year-old girl with Job syndrome, which includes immunoglobulin deficiency, had osteopenia and developed pathologic fracture of proximal tibia. She then drifted into progressive genu varum. It was felt that guided growth might not work in mechanically compromised environment.
 Patient underwent corrective osteotomy of upper tibia and fibula, supplemented with cast.
Patient underwent corrective osteotomy of upper tibia and fibula, supplemented with cast.
Fixation may be achieved with pins incorporated in a cast, with internal plating, or with an external fixator, depending on the clinical setting and the experience and personal preference of the surgeon. During the period when the bone is healing, weightbearing must be deferred, and range of motion may be limited. Physical therapy may be useful in mobilizing the patient. Fuller discussions of osteotomy techniques are available in standard orthopedic texts.
Depending upon the circumstances, surgical correction of genu varum is typically an outpatient procedure. A soft dressing usually suffices. Crutches may be used as needed for comfort and balance. Immediate range-of-motion exercise and weightbearing are encouraged. Physical therapy is provided as needed for patients who are slow to mobilize. Activities, including sports, may be resumed as tolerated.
Rebound growth and recurrent varus can occur; however, these phenomena are not predictable. Accordingly, the author does not routinely shoot for overcorrection but, rather, informs the parents before the index procedure that the child should be followed after plate removal. If no rebound effect is observed within 12 months of plate removal, then it is unlikely to occur. For rebound deformity that is clinically relevant (medial zone 2 or 3 on the radiograph), guided growth may safely be repeated.
For this meticulous but relatively simple operative procedure, complications are rare. Because minimal dissection is involved, wound-healing problems (eg, hematoma, infection, and dehiscence) are uncommon. If keloid formation is a problem, the scar may be excised at the time of plate removal.
With the switch from staples to the eight-Plate, the problems of hardware migration or fatigue have been solved. By design, the screws diverge with growth; however, this divergence does not necessitate screw exchange. The relatively thin titanium plates conform to the bone and are free to bend with correction.
Because the bone is not divided, there is no need to wait for it to heal before allowing the child to return to normal activities. Guided growth with the eight-Plate does not place the patient at risk for nonunion, delayed union, compartment syndrome, or neurologic damage, all of which have been reported with osteotomy of the distal femur or proximal tibia/fibula.
There are a number of potential and theoretical problems with the use of eight-Plates. Biologic problems include the following:
Mechanical problems include the following:
 Whereas complication rate of guided growth with eight-Plates remains low, there have been isolated cases of broken screws. Each broken screw has been distal (metaphyseal) screw in heavy-set patient with Blount disease. Potential solutions are to insert solid 4.5-mm screw or to add second eight-Plate.
Whereas complication rate of guided growth with eight-Plates remains low, there have been isolated cases of broken screws. Each broken screw has been distal (metaphyseal) screw in heavy-set patient with Blount disease. Potential solutions are to insert solid 4.5-mm screw or to add second eight-Plate.
Follow-up visits are scheduled for every 3 months. Repeat radiographs are obtained as indicated. Plate removal is carried out when the mechanical axis is neutral or minimally overcorrected into lateral zone 1 (at the surgeon’s discretion).
Follow-up is continued at 6 and 12 months after hardware removal, including a full-length anteroposterior (AP) radiograph. The parents are shown how to measure the intracondylar distance. The patient is then followed annually until maturity (ideally).
Copyright © www.orthopaedics.win Bone Health All Rights Reserved