

Despite the inherent stability of the joints of the thumb, the vulnerable anatomic position of the first phalanx often subjects the joints to mechanical strain that leads to subluxation or dislocation of the metacarpophalangeal (MCP) and interphalangeal (IP) joints. (See the image below.)
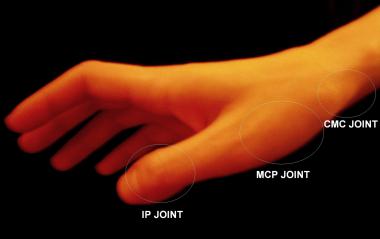 Anatomic locations of joints of thumb.
Anatomic locations of joints of thumb.
The MCP joint of the thumb is a condyloid joint that has a structurally stronger capsular ligament apparatus than the other four MCP joints of the hand do.[1] Most thumb MCP dislocations are dorsal.[2] They are caused by a longitudinal and dorsal stress along the axis of the digit that hyperextends the thumb and tears the volar plate of the joint. An example of this mechanism is a fall onto an outstretched hand (FOOSH) with an impact to the tip of an extended thumb.
Volar dislocation of the MCP joint of the thumb is comparatively rare and is associated with tears of both dorsal capsule ligaments and the extensor pollicis brevis (EPB). For this reason, anterior dislocations are often treated with surgical repair of the torn structures, and closed reduction is rarely achieved with adequate postreduction stability.
Plain film radiography is the definitive diagnostic modality for joint dislocations of the thumb, serving both to describe the geography of the dislocation and to rule out the possibility of coexisting fractures.
Intra-articular fractures should be excluded by radiology prior to attempting to reduce a joint in the thumb. These fractures include the Bennett fracture or oblique fracture through the base of the first metacarpal with dislocation of the radial portion of the articular surface.[3] The Rolando fracture is similar to the Bennett fracture except that the fracture at the base of the metacarpal is comminuted with similar dislocation of the fragments.
Dislocation of the IP joint occurs to a much lesser extent than dislocation of the MCP joint does. These injuries are most commonly dorsal and are often associated with disruption of the overlying skin and soft tissues.
Although rare cases of multiple simultaneous thumb joint dislocations, including the IP, MCP, and proximal carpometacarpal (CMC) or trapeziometacarpal (TMC) joints, have been reported in the literature, most thumb dislocations involve only a single joint.[4, 5, 6] The existence of multiple thumb joint dislocation injury underscores the necessity of careful radiographic analysis before reduction attempts are made.[7]
NextIndications for reduction of a thumb dislocation include the following:
Absolute contraindications for reduction of a thumb dislocation include the following:
Relative contraindications include the following:
Provide adequate analgesia to the injured thumb by regional injection, and, if necessary, systemic opioids. The median and radial nerves provide sensory innervation to the thumb and may be blocked as follows. (See Hand, Anesthesia.)
Median nerve blockage is accomplished by injecting 3-5 mL of 1% lidocaine without epinephrine into the nerve distribution at the volar aspect of the wrist. The area of injection is located just deep to the palmaris longus tendon or slightly radial to it, between the palmaris longus and the flexor carpi radialis tendons in a plane just proximal to the proximal palmar crease, at a depth of 1 cm or less. The needle should be inserted perpendicular to the skin and through the flexor retinaculum, but the nerve itself is actually quite superficial.
Radial nerve blockage is accomplished by injecting 2-5 mL of 1% lidocaine without epinephrine just lateral to the radial artery at the level of the proximal palmar crease and at a depth of 0.5 cm. From this initial injection site, another 5-6 mL of local anesthetic is injected in a circumferential arch around the radial half of the wrist to the dorsal midline so that the lidocaine can reach the dorsal nerve branches of the radial nerve.
Ulnar nerve blockage is not necessary for thumb joint reductions.
Equipment employed for thumb joint reduction includes the following:
Position the patient’s hand so that the radial dorsal surface is facing the physician and the hand is at approximately chest level, within comfortable reach of the physician’s grasp. This may be aided by having the patient rest his or her elbow on a firm flat surface, with the elbow flexing the hand into an upright position.
Firmly grasp the patient’s thumb either on the distal phalanx, for reduction of an interphalangeal (IP) joint dislocation, or on the proximal phalanx, for reduction of a metacarpophalangeal (MCP) joint dislocation. Use your nondominant hand to hold the patient's wrist. Keep the MCP joints of the index through small digits in comfortable extension, and maintain the wrist in passive flexion to relax the tendons.
When reducing a dorsal IP joint dislocation, hold the IP joint in gentle hyperextension. When reducing a dorsal MCP dorsal dislocation, gently hyperextend the MCP joint and actively hold it in this position. The objective is to initially exaggerate the injury.
Obtain and document a thorough preprocedural history that includes hand dominance, prior injuries, mechanism of trauma, description of presenting symptoms, subjective loss of strength or sensation, and the patient's age in reference to skeletal maturity.
Remove all rings, jewelry, or potentially constricting objects from the patient’s wrist and all digits of the patient’s hand.
Perform and document a thorough physical examination, noting ecchymoses, swelling, pallor, abrasions, lacerations, paresthesias, weakness, passive and active range of motion of the metacarpophalangeal (MCP) and interphalangeal (IP) joints of the thumb, and capillary refill of the distal nail bed.
Obtain prereduction radiographs of the hand, including adequate anteroposterior (AP), lateral, and oblique views of the carpometacarpal (CMC), MCP, and IP joints of the first digit. These allow documentation of the presence and direction of the joint dislocation while excluding the presence of a fracture of the carpals, the first metacarpal, or the first proximal or distal phalanx. In some cases, noncontrast computed tomography (CT) or magnetic resonance imaging (MRI) of the thumb may be considered.[9]
Explain the procedure, benefits, risks, alternatives, and complications to the patient or the patient’s representative, and obtain signed informed consent. Ask the patient or the patient’s representative if they would like others to be present for the procedure.
Supply appropriate anesthesia (see Anesthesia), and position the patient properly (see Positioning).
Apply appropriate forces to the injury while maintaining the established position of hyperextension, as follows.
When reducing a dorsal IP joint dislocation, apply longitudinal traction on the thumb with the hand grasping the distal phalanx. Apply simultaneous distal pressure on the dorsal base of the distal phalanx. Use your nondominant hand to hold the patient. (See the image below.)
 Position of hyperextension used for reduction of dorsal interphalangeal (IP) joint dislocation.
Position of hyperextension used for reduction of dorsal interphalangeal (IP) joint dislocation.
When reducing a dorsal MCP dislocation, do not apply initial traction on the MCP joint; doing so would increase the chance of entrapping another structure in the anatomic joint space, making reduction impossible. Instead, with your nondominant hand, apply only distal pressure to the dorsal base of the proximal phalanx. (See the image below.)
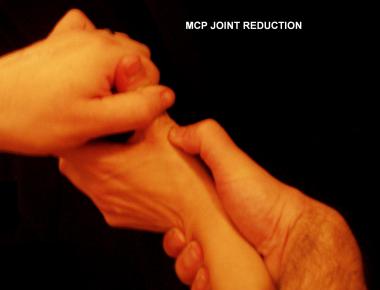 Position of hyperextension used for reduction of dorsal metacarpophalangeal (MCP) joint dislocation.
Position of hyperextension used for reduction of dorsal metacarpophalangeal (MCP) joint dislocation.
While the above forces are being applied, bring the injured joint into a position of flexion. The act of joint flexion while applying the maneuvers described above reduces the dislocation, thus resolving the injured joint’s deformity and restoring range of motion.
The joint is initially held in extreme flexion rather than hyperextension, thus exaggerating the injury.
Apply distal pressure either on the volar base of the distal phalanx (for IP dislocations) or on the proximal phalanx (for MCP dislocations). Achieve reduction by moving the dislocated joint into a position of relative extension without hyperextending the joint.
Reduction of volar MCP and IP dislocations of the thumb is less successful and leads to more complications than reduction of dorsal dislocations does.[10]
Repeat and document a complete neurovascular examination to evaluate postreduction changes in the thumb’s perfusion, sensation, and strength. Then, carefully assess and document the postreduction range of motion and stability of the injured joint.
After reducing an MCP dislocation, assess the MCP joint’s collateral ligaments by applying gentle varus/valgus pressure to the injured thumb’s proximal phalanx with the MCP joint held in flexion and documenting any joint laxity indicative of ligament rupture. Ulnar collateral ligament (UCL) rupture or gamekeeper thumb, also known as skier thumb, is of particular clinical importance in that it may indicate the presence of a Stener lesion (see Pearls). (See the image below.)
 Hand position used for testing if laxity is present with valgus strain of metacarpophalangeal (MCP) joint. Such laxity suggests presence of ulnar collateral ligament (UCL) tear and indicates possible existence of Stener lesion.
Hand position used for testing if laxity is present with valgus strain of metacarpophalangeal (MCP) joint. Such laxity suggests presence of ulnar collateral ligament (UCL) tear and indicates possible existence of Stener lesion.
If a stable reduction has not been achieved, repeat attempts may be performed; however, if the above maneuvers have been unsuccessful even when performed under optimal conditions, closed reduction should be considered impossible.
Obtain postreduction radiographs to determine and document the adequacy of reduction and reexamine for occult fractures. Radiographs should be taken even when reduction was not believed to be successful.
Apply a short arm thumb spica cast, using at least eight layers of 3-in. plaster roll. The splint should extend from the distal IP joint of the thumb to the midforearm. The distal tip of the distal phalanx of the thumb should be left exposed for serial neurovascular examination.
The splint should hold the extremity with the wrist in 20-30 º of extension and the hand in wine-glass position.
Give the patient the following instructions regarding the splint:
A follow-up appointment should be arranged with a hand surgeon or orthopedist for approximately 1 week after the reduction attempt.
Keep the MCP joint in flexion and adduction while attempting the reduction. This may aid the effort by relaxing the intrinsic muscles of the thenar eminence as well as the flexor pollicis longus.
Do not apply longitudinal traction on an MCP dislocation.
If the attempted reduction is not successful, do not make multiple repeat attempts. The volar plate, a tendon (eg, flexor pollicis longus or flexor pollicis brevis), or a sesamoid bone may be entrapped within the anatomic joint space, and reduction will be impossible without surgery.[11] Seek orthopedic consultation to schedule such a procedure.
A Stener lesion is a potential first MCP injury that would cause a reduction attempt to be unstable without operative management.[12] This type of MCP dislocation may appear identical to normal dislocations on radiographs but is complicated by a complete tear (third-degree sprain) of the ulnar collateral ligament (UCL) with displacement of the ruptured ligamentous fragment proximal to the adductor aponeurosis.
A Stener lesion can be signaled by the following findings:
 Hand position used for testing if laxity is present with valgus strain of metacarpophalangeal (MCP) joint. Such laxity suggests presence of ulnar collateral ligament (UCL) tear and indicates possible existence of Stener lesion.
Hand position used for testing if laxity is present with valgus strain of metacarpophalangeal (MCP) joint. Such laxity suggests presence of ulnar collateral ligament (UCL) tear and indicates possible existence of Stener lesion.
If a Stener lesion is suspected, immobilize the injury in a short-arm thumb spica splint, and consult an orthopedist with the goal of scheduling surgical repair of the UCL within 10 days of the injury. This injury does not heal without surgical intervention.
Patients who present with a mechanism of injury that suggests a large axial load on the thumb are more likely to have a Bennett or Rolando fracture. Particularly careful radiographic exclusion of these fractures is indicated in these patients.
Adequate closed reduction may be more difficult or impossible to achieve in the following circumstances:
Steps that may improve chances of successful reduction include the following:
Avoid increasing the strength of forces applied to the reduction attempt; this increases the potential for additional injury.
Reduction attempts, particularly if performed repeatedly and with large amounts of force, may cause neurovascular injury to the digit. This can be quickly detected by careful reexamination after each reduction attempt. If such a neurovascular injury occurs, emergency consultation with an orthopedist or hand surgeon is paramount. Surgical intervention may be the only option to reverse such an injury.
Fracture of the first metacarpal, the proximal phalanx, or the distal phalanx may occur with forceful reduction attempts. Although this is a rare occurrence, physicians should search for new fractures on postreduction radiographs, as such fractures may add a new aspect of instability to the injury.
Closed reduction may not provide adequate reduction of some Bennett fractures; the flexor pollicus longus tendon or digital nerve may block complete reduction.[13] Open reduction and internal fixation may be required.[14]
Copyright © www.orthopaedics.win Bone Health All Rights Reserved