

Osteosarcoma is the most common malignant bone tumor.[1, 2] It is an ancient disease that is still incompletely understood. Osteosarcoma is thought to arise from primitive mesenchymal bone-forming cells, and its histologic hallmark is the production of malignant osteoid. Other cell populations may also be present, as these types of cells may also arise from pluripotential mesenchymal cells, but any area of malignant bone in the lesion establishes the diagnosis as osteosarcoma.
Osteosarcoma is a deadly form of musculoskeletal cancer that most commonly causes patients to die of pulmonary metastatic disease (see the image below).[3, 4, 5, 6, 7] Most osteosarcomas arise as solitary lesions within the fastest growing areas of the long bones of children. The top three affected areas are the distal femur, the proximal tibia, and the proximal humerus, but virtually any bone can be affected.
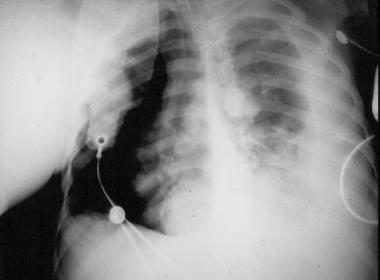 Chest radiograph of patient with osteosarcoma who died from pulmonary metastatic disease. Note the presence of a pneumothorax as well as radiodense (bone-forming) metastatic lesions.
Chest radiograph of patient with osteosarcoma who died from pulmonary metastatic disease. Note the presence of a pneumothorax as well as radiodense (bone-forming) metastatic lesions.
Not all osteosarcomas arise in a solitary fashion. Multiple sites may become apparent within a period of about 6 months (synchronous osteosarcoma), or multiple sites may be noted over a period longer than 6 months (metachronous osteosarcoma).[5] Such multifocal osteosarcoma is decidedly rare, but when it occurs, it tends to be in patients younger than 10 years.[5]
The mainstay of therapy is surgical removal of the malignant lesion. Most often, limb-sparing (limb-preserving) procedures can be used to treat patients with this disease and, thus, preserve function. Chemotherapy is also required to treat micrometastatic disease, which is present but often not detectable in most patients (~80%) at the time of diagnosis.[8]
NextOsteosarcoma is a bone tumor and can occur in any bone, usually in the extremities of long bones near metaphyseal growth plates. The most common sites are as follows:
A number of variants of osteosarcoma exist, including conventional types (osteoblastic, chondroblastic, and fibroblastic), telangiectatic, multifocal, parosteal, and periosteal. This article only addresses conventional osteosarcoma (often referred to simply as osteosarcoma).
The exact cause of osteosarcoma is unknown. However, a number of risk factors have been identified.[3, 4, 5, 6, 7, 9, 10, 11, 12, 13, 14, 15, 16]
Rapid bone growth appears to predispose persons to osteosarcoma, as suggested by the increased incidence during the adolescent growth spurt, the high incidence among large-breed dogs (eg, Great Dane, St Bernard, German shepherd), and osteosarcoma's typical location in the metaphyseal area adjacent to the growth plate (physis) of long bones.
Genetic predisposition plays a role. Bone dysplasias, including Paget disease, fibrous dysplasia, enchondromatosis, and hereditary multiple exostoses and retinoblastoma (germline form) are risk factors. The combination of constitutional mutation of the RB gene (germline retinoblastoma) and radiation therapy is linked with a particularly high risk of developing osteosarcoma, Li-Fraumeni syndrome (germline p53 mutation), and Rothmund-Thomson syndrome (autosomal recessive association of congenital bone defects, hair and skin dysplasias, hypogonadism, and cataracts).
The only known environmental risk factor is exposure to radiation. Radiation-induced osteosarcoma is a form of secondary osteosarcoma and is not discussed further in this article.
In the United States, the incidence of osteosarcoma is 400 cases per year (4.8 per million population <20 years).[17] The overall 5-year survival rate for patients diagnosed between 1974 and 1994 was 63% (59% for males, 70% for females).
The incidence is slightly higher in blacks than in whites. Data from the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER) Pediatric Monograph 1975-1995 are as follows[17] :
The incidence of osteosarcoma is slightly higher in males than in females. In males, it is 5.2 per million per year; in females, it is 4.5 per million per year.
Osteosarcoma is very rare in young children (0.5 cases per million per year in children <5 years). However, the incidence increases steadily with age, rising more dramatically in adolescence in correspondence with the adolescent growth spurt, as follows[18] :
The present understanding of outcome and prognosis for osteosarcoma is driven by certain serum markers, clinical staging, and histologic response to chemotherapeutic agents.[19]
The overall 5-year survival rate for patients diagnosed between 1974 and 1994 was 63% (59% for males, 70% for females). Patients with an elevated ALP at diagnosis are more likely to have pulmonary metastases. In patients without metastases, those with an elevated LDH are less likely to do well than are those with a normal LDH.
Bu et al conducted a meta-analysis of eight published studies to determine whether p16(INK4a) is a prognostic factor for patients with osteosarcoma.[20] The meta-analysis showed that a high level of expression of p16(INK4a) was significantly associated with favorable overall survival. The investigators concluded that p16(INK4a) is an effective biomarker of survival for patients with osteosarcoma.
Ma et al conducted a study to determine the diagnostic and prognostic value of circulating miR-148a in the peripheral blood of patients with osteosarcoma.[21] Expression of miR-148a was significantly associated with tumor size and distant metastasis. High expression of miR-148a was associated with poor overall survival and poor disease-specific survival. The investigators concluded that detection of circulating miR-148a expression in the peripheral blood is useful in identifying patients with osteosarcoma who have a poor prognosis.
A study by Zhao et al found that high expression of the oncoprotein transient receptor potential melastatin member 8 (TRPM8) was predictive of a poor prognosis in patients with osteosarcoma, in that it was associated with higher clinical stage and distant metastasis, as well as with shorter overall survival and disease-free survival.[22] TRPM8 may prove to be a useful molecular target for therapy in osteosarcoma patients.
Clinical staging as it relates to prognosis is discussed elsewhere (see Staging).
In a retrospective study by Kim et al, the records of 331 patients with stage II osteosarcoma who had undergone surgery and chemotherapy were reviewed.[23] The authors found that initial tumor size appears to be associated with histologic response and is an important prognostic factor in osteosarcoma. Other studies have shown that patients in whom a good histopathologic response to neoadjuvant chemotherapy has been achieved (>95% tumor cell kill or necrosis) have a better prognosis than those whose tumors do not respond as favorably.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved