

In 1981, Palmer and Werner introduced the term triangular fibrocartilage complex (TFCC) to describe the ligamentous and cartilaginous structures that suspend the distal radius and ulnar carpus from the distal ulna (see the image below).[1] The TFCC is the major ligamentous stabilizer of the distal radioulnar joint (DRUJ) and the ulnar carpus.
 Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. T=triquetrum; L=lunate; S=scaphoid. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. T=triquetrum; L=lunate; S=scaphoid. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Functions of the TFCC are as follows:
 Triangular fibrocartilage complex provides continuous gliding surface across entire distal face of radius and ulna to allow for flexion-extension and translational movements.
Triangular fibrocartilage complex provides continuous gliding surface across entire distal face of radius and ulna to allow for flexion-extension and translational movements.
Injuries to the TFCC present as ulnar-side wrist pain, frequently with clicking. Torn TFCCs constitute 35% of intra-articular fractures and 53% of extra-articular fractures. There is no correlation between ulnar styloid fractures and TFCC injuries. Patients with a torn TFCC display ulnar variance (radial shortening) that is on average 4.6 mm (vs 2.5 mm for no tear) and dorsal angulation of 24° (vs 12° for no tear).
Since 1777, when DeSault's original dissertation first described DRUJ injuries, much has been written about this joint and the TFCC. As Palmer pointed out,[1, 2, 3] humans are differentiated from lower primates by a radiocarpal joint with a TFCC interposed between the ulna and carpus.[1] This TFCC improves wrist functional stability and allows six degrees of freedom at the wrist—flexion, extension, supination, pronation, and radial and ulnar deviation.
As interest in the TFCC evolved, open repair techniques for this structure were devised. Small-joint arthroscopy provides the opportunity for new techniques in the debridement or repair of these structures.
NextAs the name suggest, the TFCC is triangular in shape. Palmer found an inverse relation between ulnar variance and TFCC thickness of the TFCC: The TFCC is thicker in individuals who are ulnar minus.[4] Generally, the TFCC is 1-2 mm thick at its center. This may thicken to 5 mm where the TFCC inserts into the eccentric concavity of the ulnar head and projecting styloid.
The TFCC extends ulnarly to insert into the base of the ulnar styloid (see the first image below). Distally, it inserts into the lunate via the ulnolunate (UL) ligament and into the triquetrum via the ulnotriquetral (UT) ligament (see the second and third images below), the hamate, and the base of the fifth metacarpal. Radially, the TFCC arises from the ulnar margin of the lunate fossa of the radius (see the fourth image below).
 Relation of triangular fibrocartilage complex to distal radius and ulnar styloid.
Relation of triangular fibrocartilage complex to distal radius and ulnar styloid.
 Ulnocarpal portion of triangular fibrocartilage complex (TFCC) is composed of discus articularis, ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL). Distally, TFCC inserts into lunate via ULL and into triquetrum via UTL.
Ulnocarpal portion of triangular fibrocartilage complex (TFCC) is composed of discus articularis, ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL). Distally, TFCC inserts into lunate via ULL and into triquetrum via UTL.
 Distally, triangular fibrocartilage complex inserts into lunate triquetrum via ulnolunate and ulnotriquetral ligaments. Triangular fibrocartilage complex solidly connects ulnar axis to volar carpus. Unlabeled arrow points to prestyloid recess. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Distally, triangular fibrocartilage complex inserts into lunate triquetrum via ulnolunate and ulnotriquetral ligaments. Triangular fibrocartilage complex solidly connects ulnar axis to volar carpus. Unlabeled arrow points to prestyloid recess. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
 Sigmoid notch of distal radius with distinct dorsal, palmar, and distal margins and indistinct proximal margin; triangular fibrocartilage complex arises from ulnar margin of lunate fossa of radius. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Sigmoid notch of distal radius with distinct dorsal, palmar, and distal margins and indistinct proximal margin; triangular fibrocartilage complex arises from ulnar margin of lunate fossa of radius. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Underneath the TFCC is the ulnar head. The seat, or the convex portion of the ulnar head, articulates with the sigmoid notch of the radius (see the image below). The cartilage-covered nonarticular pole of the ulnar head is deep to the articular disk.
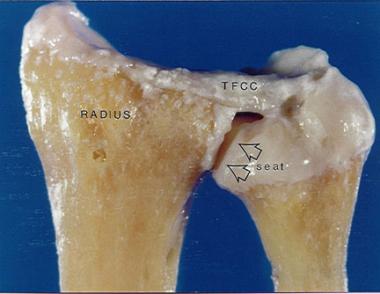 Seat of ulnar head articulates with sigmoid notch of distal radius. Radially, triangular fibrocartilage complex (TFCC) arises from ulnar margin of lunate fossa of radius. Ulnarly, TFCC inserts into base of ulnar styloid. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Seat of ulnar head articulates with sigmoid notch of distal radius. Radially, triangular fibrocartilage complex (TFCC) arises from ulnar margin of lunate fossa of radius. Ulnarly, TFCC inserts into base of ulnar styloid. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
The ulnocarpal portion of the TFCC is composed of the discus articularis and the UL and UT ligaments (referred to by some as the disk carpal ligaments). Embryologic studies have demonstrated that these ligaments arise from the disk and are critical to the carpal suspensory function of the TFCC.
The dorsal and palmar branches of the anterior interosseous artery and dorsal and palmar radiocarpal branches from the ulnar artery supply blood to the periphery of the TFCC. These vessels supply the TFCC in a radial fashion, with histologic sections demonstrating that the vessels penetrate the peripheral 10-40% of the disk. The central portion and radial attachment are avascular.
Mikic demonstrated that the percentage of the peripheral disk that is vascularized is reduced from one third in a young patient to one fourth in patients of advanced age.[5]
Because the periphery of the TFCC has a good blood supply, tears in this region can be repaired. By contrast, tears in the central avascular area must be debrided because they have no potential for healing.
The richly vascularized dorsal radioulnar (DRU) ligament and palmar radioulnar (PRU) ligament are composed of thick, longitudinally oriented collagen fiber bundles that blend in with the central avascular fibrocartilaginous portion.
When the TFCC is viewed during wrist arthroscopy, the styloid attachment appears folded. Some of the blood vessels to the TFCC enter between these folds. This fold, combined with the vascular hilum, is termed the ligamentum subcruentum, which actually is the confluence of the TFCC and the V-shaped ligament (disk ligament) as it extends from the hilar area of the styloid to its twin insertions on the lunate and triquetrum.
From a distal perspective, the TFCC has two distinct insertions into the ulna—a superficial portion and a deep portion. The superficial components, the DRU and PRU ligaments, insert into the base of the styloid. The deep portion, the ligamentum subcruentum, inserts into the fovea near the axis of forearm rotation.
A large controversy exists concerning the biomechanical changes of the TFCC during pronation and supination. A number of authors claim that the DRU ligament tightens during pronation and relaxes with supination; other authors claim the exact opposite.
Nakamura may have solved this question by using a custom-made surface coil allowing complete freedom of wrist motion. From magnetic resonance imaging (MRI) of the wrist in coronal and sagittal planes at maximal pronation and neutral and maximal supination, he showed that during pronation and supination, the TFCC twists at its origin.[6] This should result in friction between the proximal side of the disk proper and the ulnar head during rotation. The friction may increase in ulnocarpal abutment syndrome because of ulnar variance, potentially explaining the degeneration seen in Palmer class 2 TFCC tears (see Pathophysiology below).
Palmer and Werner looked at the axial load distribution through the distal radius and ulna[7] and demonstrated that with normal axial loading, 20% of the force is transmitted through the ulna and 80% through the radius. Their data also illustrated that small changes in relative ulnar length can significantly alter load patterns across the wrist. For example, with a distal radius fracture that settles 2.5 mm, an increase in ulnar axial load of approximately 40% can be expected.
Palmer, Werner, Glisson, and Murphy demonstrated that the percentage of axial force transmitted through the ulna decreases by sequential removal of the horizontal portion of the TFCC.[4] This percentage decrease is accentuated with more positive ulnar variance.
In a cadaver study, Adams demonstrated that no significant kinematic or structural changes resulted from an excision that did not violate the peripheral 2 mm of the disk and that constituted less than two thirds of the disk area.[8]
TFCC tears are associated with a positive ulnar variance. Ulnar variance increases with pronation and grip and decreases with supination.
The floor of the extensor carpi ulnaris (ECU) tendon sheath broadly connects with the TFCC. After release of the TFCC from its distal ulna attachment, Tang demonstrated a 30% increase in ECU tendon excursion during wrist extension.[9] This suggests the following:
The Palmer classification divides TFCC abnormalities into two main classes, which are then further divided into several subtypes.
Palmer class 1 (traumatic) TFCC abnormalities are categorized as follows:
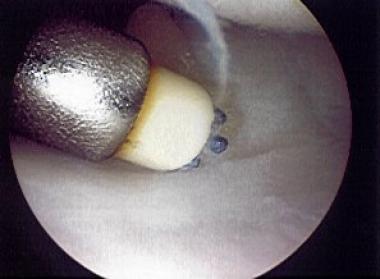
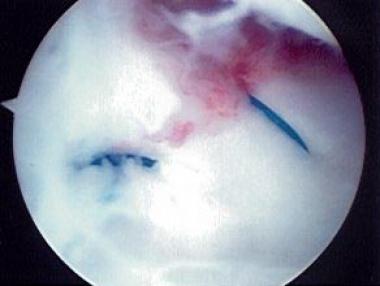
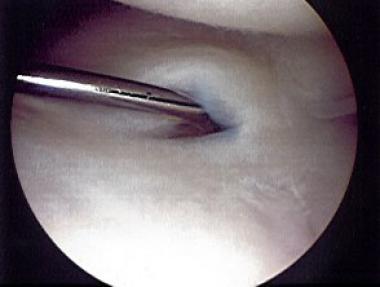 Palmer class 1A tear of triangular fibrocartilage complex that is being probed.
Palmer class 1A tear of triangular fibrocartilage complex that is being probed.
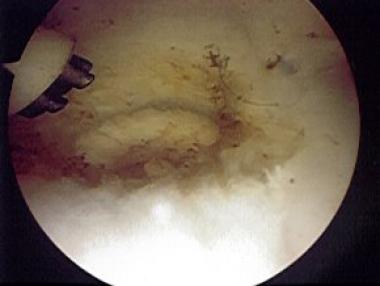
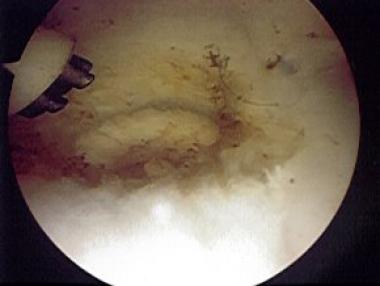
 Palmer class 1A tear of triangular fibrocartilage complex after debridement, being treated with electrothermal wand.
Palmer class 1A tear of triangular fibrocartilage complex after debridement, being treated with electrothermal wand.
 Palmer class 1A tear of triangular fibrocartilage complex after debridement with shaver and thermal treatment.
Palmer class 1A tear of triangular fibrocartilage complex after debridement with shaver and thermal treatment.
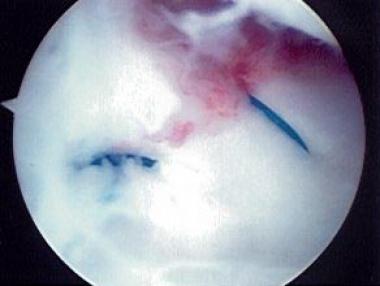
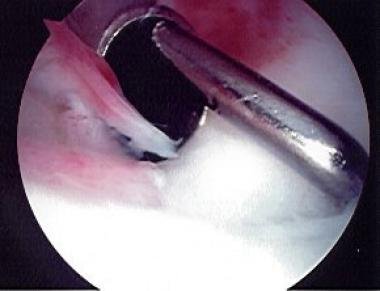 Traumatic ulnar-side Palmer class 1B tear of triangular fibrocartilage complex.
Traumatic ulnar-side Palmer class 1B tear of triangular fibrocartilage complex.
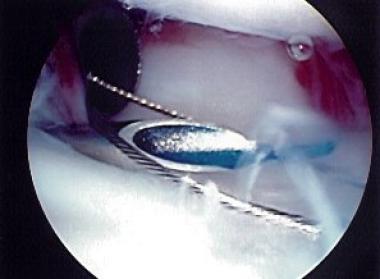 Palmer class 1B tear of triangular fibrocartilage complex treated with outside-in technique using 2-0 polydioxanone sutures and wire loop.
Palmer class 1B tear of triangular fibrocartilage complex treated with outside-in technique using 2-0 polydioxanone sutures and wire loop.
 Completion of outside-in repair for Palmer class 1B tear of triangular fibrocartilage complex.
Completion of outside-in repair for Palmer class 1B tear of triangular fibrocartilage complex.
Palmer class 2 (degenerative [ulnocarpal abutment syndrome] stage) TFCC abnormalities are classified as follows:
In a small series, Nance et al described eight patients who were presumed to have solitary TFCC tears but were found on wrist arthroscopy to have a combination of 1A and 1B injuries.[10] They suggested that this combined pattern, which is not currently categorized in the Palmer classification system and is not reliably diagnosed preoperatively, might usefully be considered a new subtype in this system.
Causative conditions for TFCC injuries include the following:
Mikic looked at 180 wrist joints in 100 cadavers, ranging in age from fetuses to 94 years.[5] He demonstrated that degeneration of the TFCC begins in the third decade of life and progressively increases in frequency and severity in subsequent decades. After the fifth decade of life, he noted no normal-appearing TFCCs. Viegas and Ballantyne found similar results.[11]
A review by de Araujo et al of 17 patients after arthroscopic repair of Palmer class IB tears, with an average patient age of 33 years, showed that at 8 months' follow-up, 16 patients (48%) were satisfied or very satisfied; one patient was not satisfied. At 16-24 months' follow-up, 70% of the patients were satisfied.[12]
Reiter et al performed a retrospective study of 46 patients who underwent arthroscopic repair of Palmer class IB tears to determine patients' functional and subjective outcomes, as well as whether clinical outcomes were related to ulnar length. Good-to-excellent results were achieved in 63% of the patients, including increased range of motion and grip strength and pain relief. Neutral or positive ulnar variance was not a contraindication for repair and did not necessitate simultaneous ulnar shortening.[13]
Sagerman and Short reviewed 12 patients after arthroscopic repair of Palmer class 1D tears, with an average follow-up of 17 months, and found good or excellent results in 67% of patients.[14]
Trumble et al reviewed 24 patients after arthroscopic repair of Palmer classes 1B, 1C, and 1D tears. The average patient age was 31 years. Treatment occurred within 4 months after injury, with a follow-up of 34 months. Postoperative range of motion was 89%, and grip strength was 85%. Thirteen of 19 patients returned to their original jobs or sports. Follow-up studies demonstrated that the TFCC was intact in 12 of 15 patients.[15]
Corso et al reviewed 44 patients (average age, 32.5 years) and 45 wrists with zone-specific repair and follow-up of 37 months and found excellent results in 29 patients, good results in 12, fair results in one, and poor results in three.[16]
In a study from 2001 through 2005 of 16 competitive athletes with wrist TFCC, McAdams et al found that arthroscopic debridement or repair of TFCC injury provided pain relief and allowed patients to return to play, with slower recovery in patients with concomitant ulnar-side wrist injuries.[8] .
Yao et al compared an all-arthroscopic TFCC repair technique with an outside-in technique in 10 matched pairs of fresh-frozen cadaveric wrists and found that the all-arthroscopic technique resulted in decreases in operating time, postoperative immobilizations, and irritation from suture knots below the skin.[17, 18]
In a study of 75 patients with TFCC repair by arthroscopic or open technique between 1997 and 2006, Anderson et al found that there was no statistical difference in clinical outcome for arthroscopic and open techniques for TFCC repair. They did note an increased rate of postoperative superficial ulnar pain in patients who underwent open repair (14/39 patients with open technique vs 8/36 patients with arthroscopy). Females had a higher rate of reoperation.[19]
In a cadaveric study comparing the biomechanical strength of knotless suture anchor repair and the traditional outside-in repair of peripheral TFCC tears, Desai et al concluded that the all-arthroscopic suture anchor TFCC repair was biomechanically stronger than the outside-in repair and that the former allowed repair of both superficial and deep layers of the articular disk directly to bone, thereby restoring native TFCC anatomy.[20] They suggested that the absence of knots might prevent irritation to the surrounding soft tissues.
Minami et al reviewed 16 patients (average age, 30 years) with a follow-up of 35 months. Palmer class 1 tears were found in 11 patients, and Palmer class 2 tears were found in five. Of the 16 patients, 13 returned to their previous jobs. Positive ulnar variance and LT tears were associated with a poor outcome; Palmer class 1 tears were associated with excellent results; and Palmer class 2 tears were associated with poor results.[21]
Westkaemper et al reviewed 28 patients (average age, 30 years) with a follow-up of 15.4 months. Excellent results were found in 13 patients, with good results in eight, fair results in two, and poor results in five.[22]
De Smet et al conducted a retrospective survey of 46 patients who underwent debridement with or without wafer distal ulna resection.[23] Patients were sent a questionnaire on pain, disability, and time off from work. Mean scores on the Disabilities of the Arm, Shoulder, and Hand (DASH) scale decreased from 42 to 28. The pain was considered severe in 12 patients; 32 patients were satisfied. There were significant differences in the outcome between use of debridement only and use of debridement with wafer resection of the distal ulna.
Minami and Kato reviewed 25 patients (average age, 32 years) with follow-up of 35 months. Ulnar variance averaged more than 3.5 mm. Ulnar-shortening osteotomies of 3 mm, fixed with a 6-hole 3.5-mm dynamic compression plate (DCP), were performed. Twenty-three patients also had arthroscopy. Palmer class 1 tears were found in 15 patients; only the flap was removed. Palmer class 2 tears were found in eight; no debridement was performed.
Complete relief or only occasional mild pain was found in 23 patients. Of the 25 patients, 23 returned to their original work. Osteotomies healed at an average of 7 weeks. This research suggests that ulnar shortening is indicated in both traumatic and degenerative tears associated with ulnar positive variance.[24]
Trumble et al reviewed 21 patients with treatment delays longer than 6 months and follow-up of 29 months. Palmer class 1 tears were repaired. Ulnar-shortening osteotomies of 2-3 mm fixed with 6-hole 3.5-mm DCPs were performed. Complete pain relief was found in 19 of 21 patients. Grip strength was 83%; range of motion was 81% of normal. Treatment delays longer than 6 months from the time of injury resulted in a higher recurrence of symptoms; in these situations, the authors recommended combining arthroscopic repair with ulnar shortening.[25]
Hulsizer et al reviewed 97 patients (average age, 34 years; average ulnar variance, 0.4 mm) with central or nondetached ulnar peripheral tears initially treated with debridement. Persistent pain more than 3 months after surgery was reported by 13 patients. A 2-mm ulnar-shortening osteotomy, fixed with a 6-hole 3.5-mm DCP, was performed on these 13 patients. Complete pain relief at 2.3-year follow-up was reported by 12 of the 13 patients. An ulnar-shortening osteotomy of 2 mm was recommended for patients in whom arthroscopic debridement failed.[26]
In a retrospective study involving 256 patients, Yamanaka et al compared preoperative and postoperative TFCC thickness and TFCC angle, using magnetic resonance imaging (MRI) to quantitatively evaluate the effect of ulnar-shortening osteotomy on disk regeneration and the suspension effect on the TFCC.[27] They found that ulnar-shortening osteotomy yielded a high residual potential for regeneration in the disk proper. There was no correlation between disk regeneration or the suspension effect on the TFCC and the Mayo wrist score.
Seo et al assessed the results of arthroscopic peripheral repair (n=15) against those of arthroscopic debridement (n=16) for treatment of chronic unstable TFCC tears in 31 ulnar-positive patients undergoing ulnar-shortening osteotomy (minimum follow-up, 24 months).[28] Improvements were noted in both groups; however, grip strength, DASH, and Patient-Rated Wrist Evaluation (PRWE) scores were better in the repair group than in the debridement group. Recovery from DRUJ instability noted during preoperative evaluation was superior in the repair group as well.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved