

In 1863, separation of the odontoid process from the body of the axis was first described in a postmortem specimen. In 1886, Giacomini coined the term os odontoideum for this condition.[1] This entity is clinically important because a mobile or insufficient dens renders the transverse atlantal ligament (TAL) ineffective at restraining atlantoaxial motion. Translation of the atlas on the axis may compress the cervical cord or vertebral arteries.[2]
Os odontoideum is rare, but the exact frequency is unknown. Many cases are incidentally detected. Others are diagnosed when patients become symptomatic. There are occasional reports of patients with os odontoideum becoming quadriparetic after minor trauma.[3, 4] To date, no large-scale screening studies have been performed. In one MRI study of odontoid morphology, a 0.7% (1 case of 133 patients) incidence was reported.[5]
An image depicting os odontoideum can be seen below.
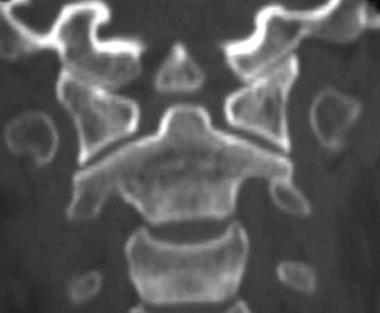 A coronal reconstruction of an orthotopic os odontoideum. Note the wide gap between the rounded ossicle and the base of the axis.
A coronal reconstruction of an orthotopic os odontoideum. Note the wide gap between the rounded ossicle and the base of the axis.
The age at diagnosis varies significantly from the first to the sixth decade of life. With increased awareness, however, os odontoideum has been diagnosed in younger patients. While the etiology remains controversial, an increased frequency of os odontoideum has been reported in patients with Morquio syndrome,[6, 7] multiple epiphyseal dysplasia, and Down syndrome.
NextInitially, os odontoideum was thought to represent a congenital failure of fusion of the dens to the remainder of the axis. As such, the condition is usually grouped with other craniocervical junction abnormalities, such as dental aplasia and hypoplasia.[12, 13, 14, 15, 16, 17, 18, 19] Today, it seems clear that failure of the secondary ossification center of the dens to fuse with the base of the odontoid represents a separate entity known as persistent ossiculum terminale.[20]
Differentiation between os odontoideum and persistent ossiculum terminale is clinically critical. The ossicle of the ossiculum terminale is much smaller than that of the os odontoideum. More important, that ossicle lies at the level of the atlantal ring above the transverse atlantal ligament. In this cranial location, ossiculum terminale, unlike os odontoideum, is not associated with significant instability.
Some authors speculate that os odontoideum represents a previous fracture of the odontoid synchondrosis before its closure at age 5-6 years.[21, 22, 23] These authors describe os odontoideum in patients with previously normal cervical radiographs. For example, Schuler et al elegantly described the evolution of an os odontoideum following trauma in a child.[24] More recently, Menezes identified os odontoideum in children younger than 5 years with a previously normal odontoid. He associated the os with unrecognized fractures.[25]
In this model, os odontoideum develops gradually. Following a fracture of the odontoid synchondrosis, with growth, the alar ligaments carry the dens fragment away from the axis base. The cranial portion of the dens fragment continues to receive a blood supply from the vascular arcade. The avascular caudad portion resorbs, leaving the characteristic rounded ossicle.
A recent paper documents os odontoideum formation after a fracture with serial radiographs.[26] Another report, in a 4-year-old girl, showed an incompletely ossified, cartilaginous orthotopic os.[27] The authors argued for a multifactorial etiology related to the embryology and vascular supply of the odontoid process. A case from the year before made a similar argument with a post-trauma CT scan showing no fracture, followed by os odontoideum 10 years later.[28]
Authors who favor a congenital basis for os odontoideum point out that the craniovertebral junction is one of the most common sites for malformation. Included are clefts or aplasia of anterior and posterior arches of atlas.[12, 15, 16, 23] On the other hand, unlike most congenital malformations, os odontoideum tends to occur as an isolated entity without other regional anomalies.[29] Garg et al reported a case of os odontoideum in a myelopathic 16-year-old patient with bipartite atlas. They concluded that coexistence of these conditions support the embryologic basis for os odontoideum. In this case, the dens had an “unusual bony projection” on its anterior surface.
Crockard and Stevens reviewed the embryologic and comparative anatomy data of clinical syndromes associated with craniocervical instability. They concluded that os odontoideum is the product of excessive movement at the time of ossification of the cartilaginous dens and is analogous to the unfused type II odontoid fracture. True hypoplasia of the odontoid peg, on the other hand, was found to be part of a wider segmentation defect associated with Klippel-Feil syndrome,[30] occipitalized atlas, or basilar invagination and rarely was found to be associated with instability.[31]
In 2006, Sankar and colleagues reviewed 519 consecutive patients with radiographic abnormalities in the occipito-cervical region. Os odontoideum was confirmed in 16. Only 3 of those patients had a history of remote trauma. The authors concluded that this supported an embryologic basis for the condition.[32]
The size of the os odontoideum may vary, but it typically is smaller than the normal dens, particularly at its base. Perhaps there are 2 etiologic groups. Certainly, in patients with other congenital anomalies or odontoid malformations, an embryologic basis may be assumed. Unfortunately, individual correlations do not “prove” the case one way or the other. A report of 3 cases of os odontoideum was reported in 2011.[33]
Regardless of the underlying cause, sound treatment selection requires an understanding of the natural history of this process. It is known that in a subset of patients, the secondary ligamentous restraints become lax. With increasing laxity, anterior motion of the atlas on the axis can become excessive. When the instability has been longstanding, it becomes multidirectional. Less clear are the percentages and rates of progression to instability. As no population studies are available, assumptions are made from case series data of nonoperatively managed patients.
Two types of os odontoideum are described, based on the position of the dens tip: orthotopic and dystopic os odontoideum. In the orthotopic type, the dens fragment lies in anatomic position. In dystopic os odontoideum, the dens tip is in any other position. Most commonly, the fragment is located near the foramen magnum, where it may fuse with the clivus. Alternatively, the os may be fixed to the anterior ring of the atlas.
Subluxation and instability are described in both types of os odontoideum. Some authors believe that dystopic os odontoideum is more likely to be symptomatic.
A significant but unknown percentage of those with os odontoideum remain asymptomatic. In this population, os odontoideum may be detected incidentally after screening or after an unrelated trauma. Given the frequency of asymptomatic os odontoideum, when symptoms do occur, it is difficult to determine with certainty that the os odontoideum is the true cause. Symptoms of os odontoideum may include:
More rarely, patients may present with thoracic pain only.[34]
In patients with cervical instability, hypermobility of C1 on C2 may lead to direct compression on the spinal cord or embarrassment of its blood supply. As a result, neurological symptoms may develop.[35, 36] These neurologic symptoms range from a transitory episode of diffuse paresis following trauma to progressive myelopathy to complete spinal cord injury.[37] Weakness and ataxia usually predominate over sensory changes.
Less frequently, atlantoaxial instability results in vertebral artery compression precipitating neurovascular symptoms. These vascular symptoms arise from the cervical cord and brainstem ischemia and encompass a bewildering array of signs and symptoms. Early sequelae include ataxia, syncope, vertigo, and visual disturbances. Later, cerebellar and brainstem infarcts and seizures are seen.[38, 39] In one recent report, onset of Ondine’s Curse (central hypoventilation syndrome) in an 18-year-old was ascribed to os odontoideum. Sudden death is rare but can occur.[40]
When os odontoideum is suspected, a thorough physical examination is mandatory. Begin with a complete neck and cervical spine examination. Evaluate for tenderness, range of motion (ROM), and associated anomalies. A careful neurologic examination should include assessment of cerebellar and brainstem function, gait evaluation, and Romberg test. In patients with atlantoaxial instability, upper motor neuron findings are commonly identified and may include spasticity, hyperreflexia, clonus, and proprioceptive loss.
Successful treatment of os odontoideum requires an understanding of the unique anatomic characteristics of the cervicocranium (occiput-C2). The bony elements here develop through enchondral ossification.
The tip of the dens and its associated ligaments arise from the fourth occipital through the cervical-0 (C0) somites, which do not ossify until middle childhood.[8, 9] The base of the dens forms from the C0 and C1 sclerotomes as 2 paired structures that ossify just before birth. The C2 and C3 sclerotomes give rise to the body of the axis, which fuses with the dens at age 4 years. The axis is shown in the image below.
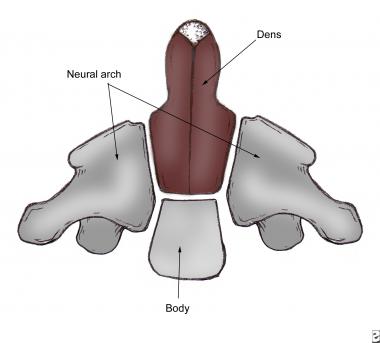 The axis has 5 primary and 2 secondary ossification centers. C0, C1, and C2 sclerotomes contribute to various portions of the dens. The principal portion of the dens body arises from the original center of C1.
The axis has 5 primary and 2 secondary ossification centers. C0, C1, and C2 sclerotomes contribute to various portions of the dens. The principal portion of the dens body arises from the original center of C1.
In a study of human embryos at 8 weeks of gestation, O’Rahilly et al reported that no transverse segmentation formed within the odontoid process at any time. An embryologic anomaly characterized by a complete/partial segmentation of 2 rostral parts will result in bipartite dens rather than an os odontoideum.[10]
The atlantoaxial joint (C1-C2) consists of biconcave articulations with loose capsules and small contact areas. Stability is therefore conferred by associated ligaments, including the TAL, which is the primary restraint to flexion and extension. Other important restraints include the apical ligaments, the alar ligaments, the tectorial membrane, and the atlanto-occipital membranes
The vertebral arteries are intricately invested in the bony anatomy of the atlantoaxial segment. They pass just inferior to the C1-C2 facet joint, then course laterally through the transverse foramen of C2. Just above the C1 lateral mass, they turn medially and meet to progress cephalad into the foramen magnum.[11] Aberrancy of the vertebral artery course is not rare and may limit fixation options in some patients selected for operative management of os odontoideum. This deviant course may be unilateral or bilateral.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved