

In growing children, sprains and strains often result in potentially serious growth plate fractures and physeal fractures (see the image below). These same sprains and strains in active adults are relatively benign injuries. This article discusses some of the important orthopedic history relative to the physes, relevant anatomy, classification systems, and some details of physeal fractures in specific areas of the body.
 Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
See Common Pediatric Sports and Recreational Injuries, a Critical Images slideshow, to help recognize some of the more common injuries and conditions associated with pediatric recreational activities.
NextIn the 1500s, Ambroise Pare made the earliest known reference to what is now known as the growth plate when he described the "appendices" of long bones. What Pare called dislocations of these appendices are now called growth plate fractures.
In 1727, Stephen Hales deduced the specific location of the growth plate. He noted that the distance between drill holes he made in the diaphyses of leg bones of chickens did not increase as the birds grew. From this, Hales correctly concluded that longitudinal growth occurred at the ends of these long bones and not in the middle.
Less than 10 years later, the study of the growth plate took a big step forward when John Belchier introduced the scientific community to an important bone-staining method using the plant product called madder. The use of madder (Rubia tinctorum) actually dates back to biblical times, when it was used as a red dying agent for clothing. Belchier noted that the bones of madder-fed animals stained red in their growth areas.
Belchier's discovery led to the extensive madder dye experiments conducted by John Hunter during the late 1700s. Hunter studied growing chickens and clearly demonstrated that longitudinal bone growth occurred because of new bone generated by the physes at the ends of long bones. Hunter is frequently referred to as the father of the growth plate because he was the first to study it in such detail.
Growth plate (physeal) fractures may be defined as disruptions in the cartilaginous physis of long bones that may or may not involve epiphyseal or metaphyseal bone.
Injuries to the physes are more likely to occur in an active pediatric population, in part because of the greater structural strength and integrity of the ligaments and joint capsules than of the growth plates. These binding ligamentous structures are two to five times stronger than the growth plates at either end of a long bone and, therefore, are less often injured in children sustaining excessive external loads to the joints.
Growth plate injuries are classified in many ways. Poland earned credit for one of the first systems in 1898; his 4-part classification system progressed from a simple epiphyseal separation to an epiphyseal separation in which it is split in two.
Many other classification systems followed, including a system suggested by Petersen in 1994. This system was constructed on the basis of a population-based epidemiologic study and arranged from the physis least involved progressing to the injury that posed the greatest threat to the physis.
Of the various classification systems have been used throughout the world, the Salter and Harris (SH) classification, initially proposed in 1963 by Robert Salter and W Robert Harris of Toronto,[1] is generally preferred and is the accepted standard in North America to facilitate communication among health care professionals.[2, 3] The SH system categorizes the various fracture patterns into six types as follows.
An SH I fracture typically traverses through the hypertrophic zone of the cartilaginous physis, splitting it longitudinally and separating the epiphysis from the metaphysis. When these fractures are undisplaced, they may not be readily evident on radiographs because of the lack of bony involvement. In many instances, only mild-to-moderate soft-tissue swelling is noted radiographically.
Clinical findings may be impressive (see the first image below); however, subsequent radiographs may demonstrate physeal widening or new bone growth along physeal margins, indicating the presence of a healing fracture (see the second image below). In general, the prognosis for this type of fracture is excellent. Usually, only closed reduction is necessary for displaced fractures; however, open reduction and internal fixation may be necessary if a stable satisfactory reduction cannot be maintained.
 Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
 Growth plate (physeal) fractures. Anteroposterior radiograph of the knee of the patient in the previous image. Note subtle physeal widening confirming the diagnosis of a Salter-Harris I fracture of the distal femur.
Growth plate (physeal) fractures. Anteroposterior radiograph of the knee of the patient in the previous image. Note subtle physeal widening confirming the diagnosis of a Salter-Harris I fracture of the distal femur.
An SH II fracture splits partially through the physis and includes a variably sized triangular bone fragment of metaphysis (see the image below). This fragment is often referred to as the Thurstan Holland fragment in honor of the British radiologist, Charles Thurstan Holland, who drew attention to its existence in 1929.
 Growth plate (physeal) fractures. Anteroposterior ankle radiograph demonstrating an impressively displaced Salter-Harris II fracture of the distal tibial epiphysis (along with comminuted fracture of distal fibular diaphysis).
Growth plate (physeal) fractures. Anteroposterior ankle radiograph demonstrating an impressively displaced Salter-Harris II fracture of the distal tibial epiphysis (along with comminuted fracture of distal fibular diaphysis).
Periosteum on the side of the Thurstan Holland fragment often remains intact, thus facilitating reduction. This particular fracture pattern occurs in an estimated 75% of all physeal fractures, and it is the most common physeal fracture. The image below illustrates an SH II fracture of the distal femur.
 Growth plate (physeal) fractures. Displaced Salter-Harris II fracture of the distal femur. The large Thurstan Holland (metaphyseal) fragment may serve an important fixation point for either a Steinmann pin or a lag screw.
Growth plate (physeal) fractures. Displaced Salter-Harris II fracture of the distal femur. The large Thurstan Holland (metaphyseal) fragment may serve an important fixation point for either a Steinmann pin or a lag screw.
An SH III fracture pattern combines physeal injury with an articular discontinuity. This fracture partially involves the physis and then extends through the epiphysis into the joint. It has the potential to disrupt the joint surface. This injury is less common and often requires open reduction and internal fixation to ensure proper anatomic realignment of both the physis and the joint surface. Poland included a fracture pattern similar to this in his scheme, in which both epiphyseal pieces were seen as free-floating fragments separated from the metaphysis.
The image below depicts a common SH III fracture of the distal tibia, a Tillaux fracture, on computed tomography (CT).
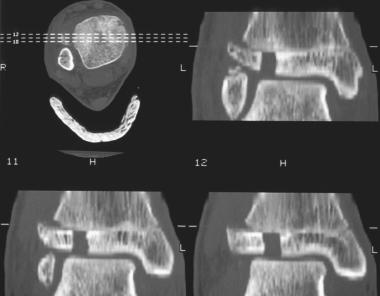 Growth plate (physeal) fractures. Multiple computed tomography (CT) scan images depicting a displaced Salter-Harris III fracture of the distal anterolateral tibial epiphysis (ie, Tillaux fracture).
Growth plate (physeal) fractures. Multiple computed tomography (CT) scan images depicting a displaced Salter-Harris III fracture of the distal anterolateral tibial epiphysis (ie, Tillaux fracture).
A SH IV fracture runs obliquely through the metaphysis, traverses the physis and epiphysis, and enters the joint. Good treatment results for this fracture are considered to be related to the amount of energy associated with the injury and the adequacy of reduction. The Thurstan Holland sign (ie, a Thurstan Holland fragment) is also seen with this fracture pattern. The image below illustrates such a fracture of the proximal tibia.
 Growth plate (physeal) fractures. Displaced Salter-Harris IV fracture of the proximal tibia. The lateral portion of the epiphysis (with the Thurstan Holland fragment) and the medial portion of the epiphysis are independently displaced (ie, each are free-floating fragments).
Growth plate (physeal) fractures. Displaced Salter-Harris IV fracture of the proximal tibia. The lateral portion of the epiphysis (with the Thurstan Holland fragment) and the medial portion of the epiphysis are independently displaced (ie, each are free-floating fragments).
A SH V lesion involves compression or crush injuries to the physis and is virtually impossible to diagnose definitively at the time of injury. Knowledge of the injury mechanism simply makes one more or less suspicious of this injury. No fracture lines are evident on initial radiographs, but they may be associated with diaphyseal fractures. (See the images below.)
 Growth plate (physeal) fractures. The Salter-Harris V fracture pattern must be strongly suspected whenever the mechanism of injury includes significant compressive forces. This is the initial injury radiograph of a child's ankle that was subjected to significant compressive and inversion forces. It demonstrates minimally displaced fractures of the tibia and fibula with apparent maintenance of distal tibial physeal architecture.
Growth plate (physeal) fractures. The Salter-Harris V fracture pattern must be strongly suspected whenever the mechanism of injury includes significant compressive forces. This is the initial injury radiograph of a child's ankle that was subjected to significant compressive and inversion forces. It demonstrates minimally displaced fractures of the tibia and fibula with apparent maintenance of distal tibial physeal architecture.
 Growth plate (physeal) fractures. Follow-up radiograph of the ankle of the child in the preceding image. This radiograph depicts growth arrest secondary to the Salter-Harris V nature of the injury. Note the markedly asymmetric Park-Harris growth recovery line, indicating that the lateral portion of the growth plate continues to function and the medial portion does not.
Growth plate (physeal) fractures. Follow-up radiograph of the ankle of the child in the preceding image. This radiograph depicts growth arrest secondary to the Salter-Harris V nature of the injury. Note the markedly asymmetric Park-Harris growth recovery line, indicating that the lateral portion of the growth plate continues to function and the medial portion does not.
SH V fractures are generally very rare; however, family members should be warned of the potential disturbance in growth and that, if growth disturbance occurs, treatment is still available (depending on the child's age and remaining growth potential).
An additional classification of physeal fractures that was not considered in the original SH classification but is now occasionally included is SH VI, which describes an injury to the peripheral portion of the physis and a resultant bony bridge formation that may produce considerable angular deformity.[4] (See the images below.)
 Growth plate (physeal) fractures. Mortise radiograph demonstrating somewhat subtle physeal injury to distal tibia. The Salter-Harris VI pattern may be suspected based upon history and physical examination findings. In this case, the radiograph indicates that it is quite likely that a small portion of the peripheral medial physis (as well as a small amount of adjacent epiphyseal and metaphyseal bone) has been avulsed.
Growth plate (physeal) fractures. Mortise radiograph demonstrating somewhat subtle physeal injury to distal tibia. The Salter-Harris VI pattern may be suspected based upon history and physical examination findings. In this case, the radiograph indicates that it is quite likely that a small portion of the peripheral medial physis (as well as a small amount of adjacent epiphyseal and metaphyseal bone) has been avulsed.
 Growth plate (physeal) fractures. Clinical photograph of the patient above with the displaced Salter-Harris II fracture of the distal femur. This mechanism of injury and physical examination findings are consistent with the Salter-Harris VI physeal injury pattern. Some may also refer to this injury type as a Kessel fracture.
Growth plate (physeal) fractures. Clinical photograph of the patient above with the displaced Salter-Harris II fracture of the distal femur. This mechanism of injury and physical examination findings are consistent with the Salter-Harris VI physeal injury pattern. Some may also refer to this injury type as a Kessel fracture.
This injury was suggested by Lipmann Kessel, who described it as follows: "A rare injury of growth plate results from damage to the periosteum or perichondral ring. . . following burns or a blow to the surface of the limb, for example a run over injury."[5]
Mann and Rajmaira collected data on 2650 long bone fractures, 30% of which involved the physes.[6] Neer and Horowitz evaluated 2500 fractures to the physes (growth plate) and determined that the distal radius was the most frequently injured (44%), followed by the distal humerus (13%), and distal fibula, distal tibia, distal ulna, proximal humerus, distal femur, proximal tibia, and proximal fibula.[7]
According to a 1972 retrospective analysis of 330 acute physeal injuries or growth plate injuries seen over the course of 20 years, males were affected more than twice as often as females. Females were most frequently affected at a younger age than males (11-12 years vs 12-14 years). These findings correspond with the growth spurts (when the physes are weakest) of the respective sexes and with males' increased willingness to engage in high-risk activities. Within this population, upper-extremity injuries were more frequent than lower-extremity injuries overall.
Growth plate (physeal) fractures are typically believed to occur through the zone of provisional calcification but may traverse several zones, depending on the type of external load application. For instance, with application of compression-type loads, the histologic zone of failure is typically the provisional calcification portion of the hypertrophic zone. Shear forces may also cause failure in the hypertrophic zone. Tension forces lead to failure of the proliferative zone.
Patients with a growth plate fracture typically complain of what seems to be localized joint pain, often following a traumatic event (eg, fall or collision). Swelling near a joint with focal tenderness over the physis is usually present (see the image below).
 Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
Growth plate (physeal) fractures. Clinical appearance of the knee of a patient with a minimally displaced Salter-Harris I fracture of the distal femur. Impressive swelling was noted adjacent to the joint, but no evidence of intra-articular swelling was present. The patient was markedly tender to palpation about the distal femoral physis.
Lower-extremity injuries present as an inability to bear weight on the injured side; upper-extremity injuries present with complaints of impaired function and reduced range of motion, quite similar to ligamentous injury. Ligamentous laxity tests of the joints of the injured side may elicit pain and positive findings similar to those indicative of joint injury. (An SH III or SH IV fracture of the distal femur is the classic example.) Do not dismiss positive joint laxity test findings as only involving the related joint tissues.
SH I and SH II growth plate (physeal) injuries usually can be managed adequately with closed manipulative reduction. Upon reduction, these injuries are typically stable, and casting suffices. At times, periosteal flaps or other local tissue may interpose into the fracture site and inhibit complete reduction. This complication may necessitate surgical extraction of the tissues to enable satisfactory or anatomic reduction.[2, 8]
SH III and SH IV injuries represent disruption of the physis and the epiphysis, as well as intra-articular fracture. Intra-articular discontinuity can lead to early degenerative arthritis, and physeal discontinuity can disturb longitudinal growth. According to Bright,[8] proper management of SH III and SH IV injuries requires anatomic reduction and internal fixation to restore anatomic alignment of the joint surfaces and proper alignment of juxtaposing physeal surfaces. In many cases, nondisplaced fracture fragments have migrated subsequent to cast immobilization only.
SH V and VI injuries often result in partial or complete growth arrest (physeal bar formation). As a result, physeal bar resection may be required, or other surgical procedures may be necessary to prevent or correct deformity.[3]
Technically, two growth plates may be considered to exist in immature long bones: the horizontal growth plate (physis) and the spherical growth plate (enables epiphyseal growth). For the purposes of this article, the horizontal growth plate is addressed. The horizontal growth plate is easily seen on radiographs of most growing long bones as a horizontal radiolucent region near the end of the bone. It may also be referred to as the cartilaginous growth plate.
The physis is an organized system of tissue located at the ends of long bones, consisting of an arrangement of chondrocytes surrounded by a matrix consisting of proteoglycan aggregates. The chondrocytes of the physis are divided into a system of zones based on different stages of maturation in the endochondral sequence of ossification and their function, as follows:
The metaphysis, adjacent to the physis, is composed of primary and secondary spongiosa layers. Primary spongiosa is mineralized to form woven bone and is subsequently remodeled to form secondary spongiosa. Branches of the metaphyseal and nutrient arteries enter the secondary spongiosa and form closed capillary loops in the primary spongiosa.
The periphery of the physis consists of two elements: the groove of Ranvier and the perichondrial ring (of Lacroix). The groove of Ranvier is a wedge-shaped zone of cells contiguous with the epiphysis at the periphery. It supplies chondrocytes to the periphery of the physis, enabling lateral growth or increased width of the physis. Langenskiold proposed that cells from the reserve zone migrate into the region of the groove of Ranvier.[9]
The perichondrial ring is a dense fibrous ring that surrounds the physis and is critical to the overall stability of the growth plate. The perichondrial ring's stabilizing effect may be lost in pathologic conditions such as slipped capital femoral epiphysis (SCFE).
Absolute contraindications to reduction of displaced growth plate fractures are few. They amount to the unusual situations in which the risks of sedation or general anesthesia are believed to dramatically outweigh the potential benefits of growth plate fracture reduction.
Relative contraindications to growth plate fracture reduction would be SH I or II fractures with clinically insignificant displacement. Also, fractures with perhaps somewhat greater displacement that present in a delayed fashion (perhaps 3 weeks or so after injury) are contraindications. In such cases, the risks of the additional force that would have to be exerted on the growth plate must be weighed against the likelihood of spontaneous remodeling of the fracture over time.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved