

Injuries of the subaxial cervical spine (C3-7) are among the most common and potentially most devastating injuries involving the axial skeleton. Assume a cervical spine injury is present until proven otherwise in patients presenting to an emergency facility with a history of a high-speed motor vehicle accident, significant head or facial trauma, a neurologic deficit, or neck pain. While assessment of airway, breathing, and hemodynamic stability continue to be the highest priority in caring for the patient with multiple traumatic injuries, central nervous system evaluation follows closely behind. The central nervous system assessment begins in the field; the cervical spine is protected until workup proves that it is not injured.
The age distribution of patients presenting with lower cervical spine and spinal cord injuries is bimodal. Injuries in persons aged 15-24 years are usually the result of high-energy trauma, such as motor vehicle accidents, accidents resulting from sporting activities, or acts of violence.[1] Injuries in persons older than 55 years usually result from low-energy trauma, such as falls from the standing position. The age-associated cervical spondylosis narrows the spinal canal and predisposes the cervical cord to injury at this level.[2]
An image depicting a lower cervical spine fracture can be seen below.
 Lateral film of a C5 burst/teardrop fracture.
Next
Lateral film of a C5 burst/teardrop fracture.
Next
The Edwin Smith papyrus (2800 BCE) referred to spinal cord injury as a disease not to be treated. Galen, in 177 CE, reported on his experiments in animals, and he described loss of movement and sensibility below the level of cord transection until breathing stopped at higher levels. Charles-Edouard Brown-S é quard did experimental work on hemisection of the cord and described his findings in papers in 1850-1851.
Operative stabilization of the cervical spine was introduced by Hadra in 1891, when he wired the spinous processes of a child who had a fracture dislocation with progressive neurologic deterioration. This was the first surgical procedure of its kind recorded in the literature. Further refinement in the application of internal fixation was documented by Rogers in 1942 with a simple wire technique, and by Bohlman with the use of triple wire stabilization. Rogers reported successful fusions in 37 of 39 patients with 1-12 years of follow-up. Bohlman's technique involved using separate wires for fixation of the adjacent spinous processes and compression of two corticocancellous grafts against the spinous processes. Biomechanically, this was thought to provide better flexural and torsional stiffness than Rogers' simple wiring. Weiland and McAfee reported 100% fusion rates in 60 patients using this means of fixation in the subaxial cervical spine.
Roy-Camille pioneered the use of posterior cervical plates to manage a variety of injuries involving the posterior subaxial spine. Magerl, Anderson, and An have proposed variations of screw insertion techniques. Anterior spinal reconstructions evolved from the use of grafts alone (iliac crest, fibula) supported with external immobilization (halo vest), to the use of anterior instrumentation with plates and bicortical screw fixation (Caspar), to unicortical locking plates (Morscher Synthes cervical spine locking plate [CSLP] system).
Skull traction using modified ice tongs was introduced by Crutchfield in 1933. The halo device was pioneered by Nickel and Perry in the late 1950s, primarily to immobilize the cervical spine affected by polio. Its application was extended to trauma cases, providing a better means of immobilization.
The cervical spine often is injured in motor vehicle accidents and falls, resulting in bony or soft-tissue injury; however, the presence of multiple traumatic injuries may distract the examiner from the cervical spine. When evaluating the polytrauma patient, examining the cervical spine is a high priority and must take precedence in the evaluation.
The cervical spine is important to consider in positioning the head in space. The dominant motion in the lower cervical spine is flexion-extension, but the cervical spine's anatomy permits a fair amount of motion in all planes. In high-speed injuries, the head can act as a significant lever arm on the cervical spine and, depending on the mechanism, can create a wide array of injury patterns.
The lower cervical spine can suffer minor bony or ligamentous injury that nevertheless results in severe neurologic injury. However, the converse is also true: major bony or ligamentous injury to the lower cervical spine can present with only neck pain. Thus, a thorough and orderly approach to the examination is paramount. Recognizing injury to the lower cervical spine is important because of the association between these injuries and spinal cord and nerve root injury. Little room for malalignment exists in the lower cervical spine, and safe and expedient realignment is of the utmost priority.
Cervical spine injury has been reported in 2-4.6% of patients presenting with blunt trauma. It is the most devastating musculoskeletal injury and occurs most frequently in young patients. Spinal cord injury occurs in more than 11,000 patients per year, or in 40-50 persons per million population. Injuries to the cervical spine produce neurologic damage in approximately 40% of patients. In approximately 10% of traumatic cord injuries, radiographs reveal no obvious evidence of bony abnormality.
Motor vehicle accidents, falls, and accidents resulting from recreational activities are the leading causes of injuries to the lower cervical spine. Motorcycle accidents account for approximately 20% of motor vehicle accidents leading to spinal cord injuries. The incidence of falls leading to injury is higher in older persons (those aged 65 y and older). Spinal injuries have increased among skiers and snowboarders.[3]
Various mechanisms may be responsible for ligamentous and bony failure in the subaxial cervical spine. The importance of the position of the head and neck at the time of impact and the direction of force causing injury cannot be overemphasized. Clinical examination and critical review of the imaging studies help to determine the type of failure and, therefore, the reconstruction required.
Conceptually, the cervical spine may be viewed as being composed of 2 columns. An anterior load-bearing structure consists of all structures anterior to and including the posterior longitudinal ligament. The posterior column includes the pedicles, laminae, facet joints, spinous processes, and the posterior ligament complexes (ligamentum flavum, interspinous ligaments, and supraspinous ligaments). Tension is resisted by the posterior column, which fails under extreme flexion or distraction and which may be associated with concomitant injury to the anterior column.
Allen and colleagues introduced a comprehensive classification system of injuries.[4] This classification system includes 3 common mechanisms: compression-flexion, distraction-flexion, and compression-extension. Vertical compression injury results in the burst-type injury with anterior column failure. Less common modes of insult are the distraction-extension and lateral flexion subtypes. These are classified further into stages of progressive injury.[5]
Fracture or dislocation of the cervical spine should be suspected in any patient involved in a high-velocity injury. Successful treatment starts with appropriate transportation of the patient from the scene of the accident to the trauma center. Airway, breathing, and circulation should always be the highest priority. Immobilization of the cervical spine with sandbags or a cervical collar and placement of the patient on a long spine board help to prevent secondary injury. Transfers and intubation should be accomplished under strict spine precautions.
An initial history should be taken, and mental status and consciousness level should be assessed. Important points to note are whether the patient was thrown from the vehicle, whether the patient hit his or her head, and whether any indication of paralysis was present at the time of the accident. Voluntary actions, neurologic function, and regions of pain also should be noted. The patient should be inspected thoroughly for lacerations or abrasions on the scalp, face, neck, or shoulders as clues to the mechanism of injury. The back of the neck should be palpated for any tenderness, step-off, or hematoma.
A thorough neurologic examination should be performed as soon as possible to detect any evidence of cord damage. It should follow the standards established by American Spinal Injury Association (ASIA). Motor strength is graded 0-5 in all major myotomes.
A systematic sensory examination is performed to detect light touch, pinprick, and proprioception in all key dermatomes of the trunk and extremities. Deep tendon reflexes are recorded. These include the biceps (C5), triceps (C7), and brachioradialis (C6) for the upper extremities, along with the patella (L4) and Achilles (S1) for the lower extremities. The presence of pathologic reflexes also should be noted. Clonus is a sustained, repetitive, involuntary contraction of a major muscle group, usually seen in the Achilles and recorded as the number of "beats" or contractions sustained. The Hoffman sign is seen in the hands with forced passive flexion of the distal interphalangeal (DIP) joint of the long finger causing a reflex contraction of the flexors of the index finger and thumb. The Babinski sign is seen when the toes exhibit an upward motion as opposed to a downward motion in response to a stroking stimulus on the bottom of the foot.
Particular emphasis should be placed on the examination of the sacral roots and reflexes. These are extremely important for two reasons. First, detection of sacral sparing indicates an incomplete spinal cord injury. Second, return of the sacral reflexes indicates the passing of spinal shock. Anal sphincter tone and perianal sensation are good tests of sacral root function. The bulbocavernosus reflex and anal wink are good tests of the sacral reflex arc.
Repeating examinations serially is crucial to determine the end of spinal shock, which usually occurs in 24 hours. Serial examinations also help to determine whether an incomplete lesion is improving or worsening. This better helps to define the best treatment pathway.
The primary indications for surgical intervention in subaxial cervical injuries include malalignment of the spine, with or without neurologic deficits, and progressive neurologic deterioration in the face of persistent compression from bone or disk fragments. While malalignment can be managed initially with cervical tong traction, definitive surgical stabilization, with or without decompression, generally is required.
Anterior column trauma may result from axial loading injuries in combination with flexion, extension, or rotational moments. Typically, the burst fracture or teardrop variant occurs with translation of bony fragments into the spinal canal.[6, 7, 8] Direct trauma to the cord may result in incomplete or complete spinal cord injury syndromes. Most frequently, anterior spinal cord injury is accompanied by loss of motor function and pain and temperature sensations, along with preservation of proprioception and vibratory sensation.
Central cord syndrome refers to the clinical picture of greater upper-extremity involvement than lower-extremity motor deficits. Return of function follows a distinct pattern of lower-extremity improvement, followed by upper proximal muscle improvement, followed finally by distal upper extremity function, which may recover incompletely. Brown-Séquard syndrome is typically a hemisection of the spinal cord, with loss of ipsilateral motor function below the level of involvement; contralateral pain; and temperature loss. This is typically seen with penetrating injuries, such as gunshot wounds.
Posterior injury may result in unilateral or bilateral facet fracture, dislocation, or both. Isolated spinous process injury is usually a stable injury and does not require surgical attention. Unilateral facet dislocations may be the most difficult to reduce by closed means, and open reduction and stabilization are often necessary.[9] Radiculopathies with or without cord damage may be seen with the unilateral facet injury. Bilateral facet dislocations have the highest incidence of spinal cord injury, with both incomplete and complete syndromes appearing.
The subaxial cervical spine can conveniently be divided into anterior and posterior columns. The anterior column consists of the typical cervical vertebral body sandwiched between supporting disks. The anterior surface is reinforced further by the anterior longitudinal ligament, and the posterior body by the posterior longitudinal ligament, both of which run from the axis to the sacrum. Articulations include the disk-vertebral body, uncovertebral joints, and zygapophyseal joints. The disk is thicker anteriorly, contributing to the normal cervical lordosis, and the uncovertebral joints located in the posterior aspect of the body define the lateral extent of most surgical exposures. The zygapophyseal or facet joints are oriented 45º to the axial plane, allowing a sliding motion, as the joint capsule is weakest posteriorly. Supporting ligamentum flavum, posterior and interspinous ligaments also strengthen the posterior column.[10]
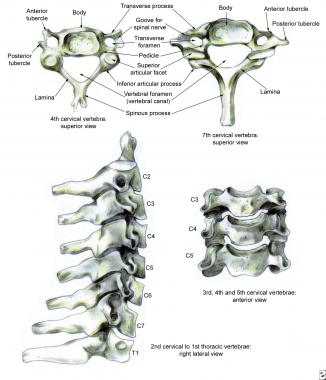 Normal anatomy of the lower cervical spine.
Normal anatomy of the lower cervical spine.
In the neuroanatomy of the cervical spine, the cord is enlarged, with lateral extension of the gray matter consisting of the anterior horn cells. The lateral dimension spans 13-14 mm, while the anterior-posterior extent measures 7 mm. An additional 1 mm is necessary for the cerebrospinal fluid anteriorly and posteriorly, as well as 1 mm for the dura. A total of 11 mm is needed for the cervical spinal cord. Exiting at each vertebral level is the spinal nerve root, which is the result of the union of the anterior and posterior nerve root.
Interconnections are present between the sympathetic nervous system and the nerve root proper. Since the numbering of the cervical roots commences above the atlas, 8 cervical roots exist, with C8 exiting between the seventh cervical vertebra and the first thoracic level.
 Cross-sectional anatomy of the cervical cord.
Cross-sectional anatomy of the cervical cord.
The vascular anatomy consists of a larger anterior spinal artery located in the central sulcus of the cord and paired posterior spinal arteries located on the dorsum of the cord. The anterior two thirds of the cord is generally accepted to be supplied by the anterior spinal artery, and the posterior one third is generally accepted to be supplied by the posterior arteries.
Reduction of subaxial malalignment must be undertaken with caution in the presence of certain concomitant disk herniations. Those that displace posteriorly and inferiorly have been reported to cause worsening neurologic deficits with both open and closed reductions. In the awake and cooperative patient, cautious reduction can be performed while performing serial neurologic examinations. In the case of intoxication or closed head injury, in which examination may be impeded, magnetic resonance imaging (MRI) may prove prudent to avoid catastrophic neurologic injury. If such a disk herniation is identified prior to reduction, it can be removed anteriorly, and reduction then can be performed safely. This has been described in both unilateral and bilateral facet dislocations.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved