

Atlantoaxial instability (AAI) is characterized by excessive movement at the junction between the atlas (C1) and axis (C2) as a result of either a bony or ligamentous abnormality. Neurologic symptoms can occur when the spinal cord or adjacent nerve roots are involved.
This instability can originate from congenital conditions, but in adults, it is primarily seen in the setting of acute trauma or degenerative changes due to the inflammatory pannus of rheumatoid arthritis (RA). Infection has been found to be an additional cause of instability, with the rich arterial supply and venous plexus in this region of the body providing a route for infectious sequelae.
Congenital causes are multiple and include Down syndrome, osteogenesis imperfecta, neurofibromatosis, Morquio syndrome, Larsen syndrome, spondyloepiphyseal dysplasia (SED), chondrodysplasia punctata, metatropic dysplasia, and Kniest syndrome. Other formative characteristics include diseases that impact bone metabolism or structure and ligament characteristics.
NextAAI may occur as a result of abnormalities or trauma associated with the C1-2 articulation, causing excessive movement around this joint. This includes the articulation between the anterior arch of C1 and the odontoid process of C2, as well as the facet joints of the posterior elements. The following three patterns are noted:
The most common abnormalities involve the transverse ligament or odontoid process.[1] The strong transverse ligament and the facet capsules maintain the integrity of the atlantoaxial articulation. The transverse ligament is the primary restraint against anterior translation of the C1 on C2, whereas the odontoid is the primary restraint against posterior translation. (See the image below.) Cadaveric studies have demonstrated that the transverse ligament is stronger in resisting anteroposterior (AP) forces before failure as compared with lateral forces.
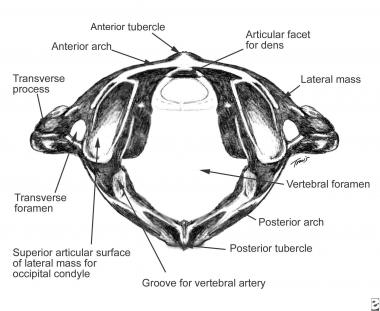 Transverse ligament holds dens against anterior arch of atlas.
Transverse ligament holds dens against anterior arch of atlas.
AAI is defined as an atlantodental (or atlantodens or atlas-dens) interval (ADI) of greater than 3 mm in adults and of greater than 5 mm in children as measured on plain radiography. The ADI is the distance between the odontoid process and the posterior border of the anterior arch of the atlas.
Symptomatic AAI occurs when subluxation or dislocation causes the odontoid process, or posterior arch of the atlas, to impinge on the spinal cord and cause neurologic manifestations. In addition, motion of the C1-2 segment can cause compression of adjacent or exiting nerve roots. No evidence exists that individuals with asymptomatic AAI are at higher risk for the development of symptomatic AAI.
Vertical displacement of the atlas requires widening of the C1-2 facet joint. The underlying problem is the disruption of the alar ligament, the superior longitudinal band of the cruciate ligament, the tectorial membrane, or a combination of these structures. (See the image below for anterior and posterior ADI landmarks.)
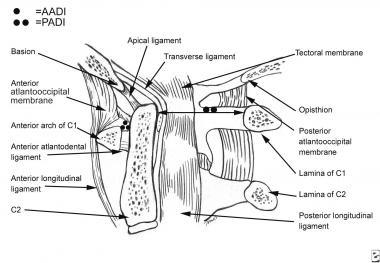 Midsagittal section of upper cervical spine. Note landmarks for measuring anterior atlantodental interval (AADI) and posterior atlantodental interval (PADI).
Midsagittal section of upper cervical spine. Note landmarks for measuring anterior atlantodental interval (AADI) and posterior atlantodental interval (PADI).
Traumatic rotatory displacement of the atlas can vary from subluxation to dislocation. The four types of atlantoaxial rotatory subluxation are shown in the image below.
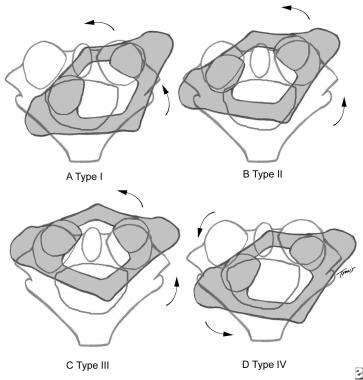 Shown are 4 types of atlantoaxial rotatory subluxation.
Shown are 4 types of atlantoaxial rotatory subluxation.
Because the cervical spine has multiple synovial-lined articulations, RA can manifest itself in the upper cervical spine.[2, 3] In a person with AAI, the rheumatoid process affects the articular cartilage of the apophyseal joints, even the type II articular cartilage in the transverse ligament.[4] In addition, the rheumatoid pannus and the associated inflammation can weaken the transverse ligaments, alar ligaments, and facet capsules early in the disease process.
With the formation of the pannus, the large excursion of C1 on C2 can cause further attenuation of the ligaments and destruction of the subchondral bone and erosion of the dens, which also contribute to the instability. Although the predominant instability is in the AP plane, lateral and rotational instability can also occur.[5]
Grisel syndrome is the occurrence of atlantoaxial subluxation (AAS) following inflammation of adjacent soft tissues after a pharyngeal infection or surgical intervention. Primarily seen in children aged 5-12 years (though possible in adults), its etiology and pathoanatomy are not totally understood. Parke demonstrated direct connection between the periodontal venous plexus and the pharyngovertebral veins.[6] This may provide a route for exudates to be transported to the cervical spine, creating a local inflammatory reaction.
In addition, children appear to be more susceptible secondary to their steeper dens-facet angle and rich vascular folds in the atlantoaxial and lateral atlantoaxial joint.
In individuals with Down syndrome, the primary cause of AAI is the laxity of the transverse ligament, which holds the dens against the posterior border of the anterior arch.
Certain other congenital conditions can be associated with AAI. These include congenital scoliosis,osteogenesis imperfecta,neurofibromatosis, Morquio syndrome, Larsen syndrome, SED congenita, chondrodysplasia punctata, metatropic dysplasia, and Kniest syndrome.
Other causes of AAI include odontoid anomalies such as aplasia, hypoplasia, duplication, third condyle, os terminale, and os odontoideum. Atlanto-occipital fusion also predisposes a patient to the development of AAI. A diagnosis of exclusion is idiopathic laxity of the transverse atlantal ligament.
AAI or AAS associated with bony abnormalities can be caused by abnormal development or ossification of the odontoid or fracture with or without remodeling. In addition, tumors can be a source of bony destruction, causing a pathologic fracture of either C1 or C2 and resulting in AAI.
The cause of AAI associated with problems of the transverse ligament is not known. An abnormal protein structure in connective tissue may cause the ligamentous laxity observed in individuals with Down syndrome. Inflammation of the ligament, as observed in persons with AAI secondary to infections or RA, can weaken the joint and predispose to subluxation.
The following conditions can be associated with AAI:
AAI is very rare in patients without predisposing factors. No data exist regarding prevalence in the absence of known risk factors. Among individuals with Down syndrome, the frequency of asymptomatic AAI was estimated to be 13.1% on the basis of a study by Pueschel et al that reviewed the radiographs of 404 patients with the syndrome.[7] Symptomatic AAI was found to be in 1.5% of these patients.
Approximately 14% of odontoid fractures have associated severe AAI, with a significant impact on patient morbidity and a twofold increase in mortality.[8]
In persons with RA, the rate of AAI or AAS has been found to be around 20%, but it has been reported to be as high as 49% in an older study population.[9, 10, 11, 12, 13, 14]
Although the introduction of biologic agents has changed the treatment of RA, the effect of such treatment on cervical lesions had not been studied until comparatively recently. In a small retrospective study of 38 patients receiving some form of biologic therapy, Kaito et al reported an 8% rate of de novo development of cervical lesions.[15, 16] There was still a high rate of disease progression in patients that were already on the spectrum of cervical disease (81%).
Unfortunately, an intervention-versus-control trial is ethically impossible in view of the known benefits of biologic therapy in other targets of rheumatoid disease; consequently, the impact of these agents on development and cervical progression has yet to be truly determined. Long-term case studies compared to historical matched controls will be required to make any further comparison.
Takahashi et al completed one such review comparing patients to historical reports and found there to be a 10-30% reduction in the prevalence of cervical spine instability in the wake of approval of the use of biologic agents; however, because of the insufficiency of the numbers, the findings were not statistically significant.[17]
No strong preponderance of AAI exists in any one age group. A higher risk does exist in younger individuals with Down syndrome (probably because of a strengthening of the transverse ligament with age) or older patients with RA (secondary to prolonged exposure to the disease process). In addition, Grisel syndrome is more prevalent in the pediatric population, but AAS can occur after any oropharyngeal infection. Most of these cases resolve and reduce spontaneously without ever presenting for treatment.
Although no sex association has been noted with idiopathic AAI, other conditions that could lead to developing this instability may be considerably more common in one sex than in the other. For example, RA affects nearly five times as many women as it does men.
No racial predilection is recognized.
Prognosis is good for patients with symptomatic AAI in whom posterior spinal fusion is successful and function returns. Surgery may relieve pain, decrease myelopathy, or both in many patients, with results depending on the severity of symptoms and the cause of instability.
Pain is the most common presenting symptom for patients with AAI or AAS. This can be either a vague neck pain or a headache. However, this pain is an extremely nonspecific finding, and these patients will require further evaluation to determine its source. The proximity of the spinal cord and vascular supply to the posterior elements can lead to additional severe effects such as myelopathy or vascular occlusion. Exact frequencies for these effects are not available, but they are understood to increase as the disease and instability progresses.
Neurologic manifestations include clumsiness, lack of coordination, abnormal gait, difficulty walking, easy fatigability, neck pain, limited next mobility, torticollis, sensory deficits, neurogenic bladder, upper motor neuron signs (spasticity, hyperreflexia, clonus, Babinski sign), paraplegia, hemiplegia, and quadriplegia. Any patient with risk factors for development of AAI merits urgent radiographic and surgical evaluation.
Mikulowski reported on the postmortem study of 104 patients with RA.[18] Cervicomedullary compression was noted in 11 patients, and seven of the 11 died suddenly. Untreated AAI in individuals with RA can have severe consequences. In addition to cervicomedullary compression, vertebral artery insufficiency has been reported as a result of the tortuous path of the artery at the atlantoaxial articulation.
It has been reported that death is common in patients with RA once myelopathy develops in the patients with cervical spine involvement. Thirty-day mortality has been reported to be as high as 13% and 60% at 4 years in patients with advanced cervical disease.[19]
Family members of pediatric patients with conditions predisposing to AAI or AAS should be aware of neurologic symptoms indicative of symptomatic progression. Discussions with the treating physician are imperative for family and patient education.
For patient education resources, see the First Aid and Injuries Center, as well as Torticollis.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved