

Children with neuromuscular disorders often manifest fixed knee flexion deformity due to muscle weakness or imbalance. They tend to develop a crouch gait pattern that may prove refractory to physical therapy, bracing, or spasticity management (Botox/baclofen)[1] ; for those children, surgical management may be indicated. In addition to hamstring recession for contracture, fixed deformities may require posterior capsulotomy or supracondylar osteotomy. Alternatively, or in addition to the above, some surgeons have resorted to external frame distraction. A new concept is to utilize guided growth of the anterior distal femur to achieve safe and gradual correction of the crouch pattern.
The image below depicts chronic fixed knee flexion deformity.
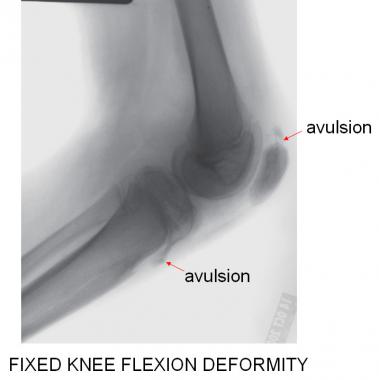 The lateral radiograph best demonstrates the open physes and the stigmata of chronic fixed knee flexion deformity (FKFD). This patient has avulsion "fractures" of the superior pole of the patella and of the tibial tubercle.
Next
The lateral radiograph best demonstrates the open physes and the stigmata of chronic fixed knee flexion deformity (FKFD). This patient has avulsion "fractures" of the superior pole of the patella and of the tibial tubercle.
Next
When evaluating sagittal knee deformity, it is important to differentiate between dynamic contracture, due to tight hamstrings, and fixed flexion deformity, which may or may not include tight hamstrings, depending upon the etiology.
The fixed knee flexion deformities (FKFD) are often insidious and recalcitrant to nonoperative management. Except for teratologic etiologies such as arthrogryposes and pterygium syndrome, where deformity may develop in utero, those due to cerebral palsy or spina bifida may not be problematic until the child reaches several years of age.[2, 3, 4, 5, 6, 7] Pain is a frequent problem, which may reflect patella alta and fragmentation of the patella, or the tibial tubercle, or both.
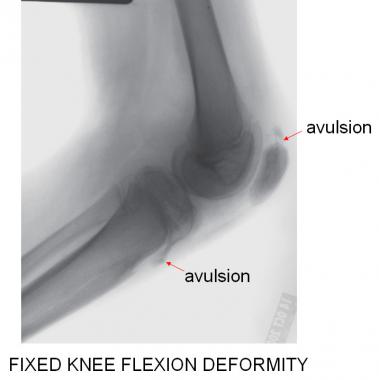 The lateral radiograph best demonstrates the open physes and the stigmata of chronic fixed knee flexion deformity (FKFD). This patient has avulsion "fractures" of the superior pole of the patella and of the tibial tubercle.
The lateral radiograph best demonstrates the open physes and the stigmata of chronic fixed knee flexion deformity (FKFD). This patient has avulsion "fractures" of the superior pole of the patella and of the tibial tubercle.
The quadriceps is relatively weak compared to the overpowering (and sometimes spastic) hamstrings. While hamstring stretching, bracing, and weakening with Botox or baclofen are in vogue for dynamic imbalance, these measures are not adequate to address fixed deformities; there may be inexorable progression of the FKFD due to growth and gravity.
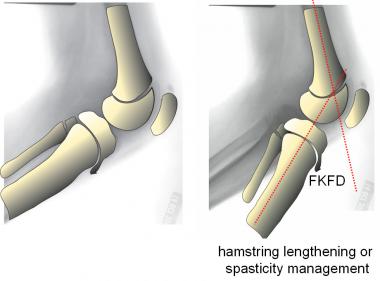 For flexion contracture, spasticity management (Botox/phenol/baclofen) or hamstring recession may offer some improvement, but these measures cannot overcome fixed knee flexion deformity (FKFD).
For flexion contracture, spasticity management (Botox/phenol/baclofen) or hamstring recession may offer some improvement, but these measures cannot overcome fixed knee flexion deformity (FKFD).
Even surgical lengthening of the hamstrings will only increase the dynamic range of knee extension (and potentially weaken hip extension), without affecting the fixed flexion component. While one may resort to posterior capsulotomy with or without posterior cruciate ligament release, this poses unnecessary neurovascular risks and may destabilize the knee.
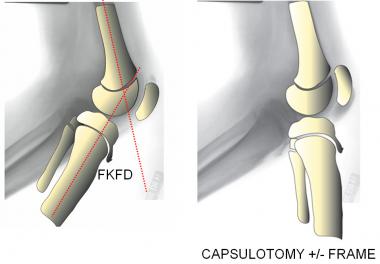 A posterior capsulotomy with or without PCL release can address fixed knee flexion deformity (FKFD), albeit with some risks, including neurovascular stretch injuries. Even with prolonged bracing following cast or frame removal, recurrent deformities are common.
A posterior capsulotomy with or without PCL release can address fixed knee flexion deformity (FKFD), albeit with some risks, including neurovascular stretch injuries. Even with prolonged bracing following cast or frame removal, recurrent deformities are common.
Once the fixed deformity surpasses 20º, braces may not be tolerated, and the child is apt lose the ability to stand and ambulate, despite attempted bracing with ankle-foot orthoses (AFOs), floor reaction braces, or even knee-ankle-foot orthoses (KAFOs).
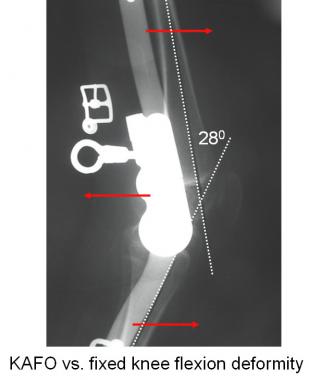 Locking KAFO may support the patient for standing but cannot adequately address FKFD. When the deformity exceeds 20º, braces are poorly tolerated.
Locking KAFO may support the patient for standing but cannot adequately address FKFD. When the deformity exceeds 20º, braces are poorly tolerated.
The problem may not be isolated to the knee; there often is concomitant hip flexion deformity that may be either fixed or dynamic, along with pseudo-equinus of the ankle. To further compound matters, there may be frontal plane knee deformities (varus or valgus) that are difficult to appreciate preoperatively, as well as torsional deformities of the long bones.
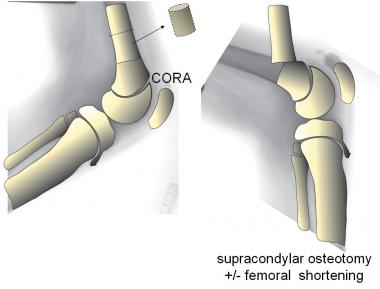
While supracondylar femoral osteotomy may render the limb straight, this produces an obligatory recurvatum of the distal femur and unsightly prominence of the patella.
 This child with arthrogryposis underwent unsuccessful posterior capsulotomies at age 3.
This child with arthrogryposis underwent unsuccessful posterior capsulotomies at age 3.
This will alter the arc of knee motion, sacrificing flexion to gain extension. There are associated fixation challenges and neurovascular risks, which are doubled in patients with bilateral involvement. As a result of continued growth, recurrent flexion deformity is all too common, requiring repeat osteotomy or frame distraction to regain knee extension. The protracted recovery time and associated costs of serial osteotomies make this a daunting challenge for both patients and caregivers.
Knee flexion contractures due to hamstring contractures and/or quadriceps weakness are prevalent in growing children with neuromuscular conditions, such as cerebral palsy, spina bifida, and arthrogryposis. A subset of these patients will develop fixed knee flexion deformity (FKFD); the frequency of FKFD is not known. It is a component of bilateral, multilevel deformities that may literally be the rate-limiting step with respect to functional ambulation.
A number of relatively common conditions, especially cerebral palsy and spina bifida, may lead to progressive fixed knee flexion deformity (FKFD), despite appropriate physical therapy and bracing. Congenital FKFD, with or without fixed lateral dislocation of the patella, may be evident on perinatal ultrasound.
Normal sagittal alignment includes the ability to lock the knee in full extension, stabilized posteriorly by the cruciate ligaments, posterior capsule, hamstrings, and gastrocnemius. This permits the child to bear full weight without pain, instability, or fatigue, because the ground reaction force is slightly anterior to the extended knee, allowing the child to lock the knee in extension during stance.
In cerebral palsy, spastic hip flexors and hamstrings combine to flex the knee, causing the ground reaction force to pass behind it and produce a flexion moment. With compromise of the hip extensors and quadriceps, gravity and fatigue force the child into a progressive crouch gait pattern.[8, 9, 10, 11] Knee pain is a frequent complaint, which may reflect fatigue of the quadriceps and/or tension failure of the patellar ligament or its bony attachments. Ankle and/or hindfoot valgus will contribute to lever arm insufficiency and further decrease the extensor moment at the knee.
Children with spina bifida often have intrinsic weakness of the quadriceps, combined with sparing or (if tethered) spasticity of the hamstrings. This puts them at risk for the same problem of fixed knee flexion deformity (FKFD) and progressive crouch gait.[11] Compounded by ankle valgus, and perhaps planovalgus of the foot, they too have lever arm dysfunction with loss of push-off strength.
Children with arthrogryposis, pterygium syndrome, and other teratologic conditions may manifest fixed knee flexion at birth, with or without congenital lateral dislocation of the patella. They often present unique challenges for the surgeon, and treatment must be individualized accordingly. The deformity may be oblique plane, including valgus or, less commonly, varus of the knee. Concurrent dislocation or stiffness of the hip and clubfoot or vertical talus may need to be addressed as well.
In the ambulatory patient, an obligatory crouch gait will be obvious, but it is not necessarily symmetrical. In the seated position, patella alta may be evident, along with reduced power of voluntary knee extension. The femoral condyles may be prominent with an empty sulcus, reflecting the proximal migration of the patella. There may be prominence and tenderness at either pole of the patella and/or over the tibial tuberosity. While there may be knee crepitance, an effusion is generally not present because of the chronic nature of the problem.
In the supine position, a straight leg raise should be evaluated. If the degree of knee flexion increases as the hip is flexed (increased popliteal angle), then a concomitant hamstring contracture is likely. If there is no change in the popliteal angle with limb elevation (a bent leg raise), then FKFD is the diagnosis.[12]
In the prone position, a torsional profile should be documented, as well as the inward-outward range, including hip rotation, and the thigh-foot axis. While the patient is prone, it is easy to look for dynamic versus fixed hip flexion deformity and rectus femoris contracture (Ely test). Also, with the hamstrings relaxed, one can discern a fixed knee flexion deformity because the ankle/foot will not rest be resting on the table.
 This ambulatory 15-year-old boy with arthrogryposis has never had an osteotomy; he was managed with stapling, followed by 8-plates, when he developed a recurrence. He has full extension on the right and 7º residual FKFD on the left. The 8-plates are still in situ (on the left) pending further growth.
This ambulatory 15-year-old boy with arthrogryposis has never had an osteotomy; he was managed with stapling, followed by 8-plates, when he developed a recurrence. He has full extension on the right and 7º residual FKFD on the left. The 8-plates are still in situ (on the left) pending further growth.
{refINDICATIONS}[[13] 13] Children with teratologic fixed knee flexion deformity (FKFD) noted in the nursery are likely to undergo surgical treatment within the first 24 months of life. Depending on the need to correct hip and foot deformities, this may be multilevel or simultaneous, or it may need to be staged. Hamstring lengthening and posterior capsulotomy may constitute the initial treatment.[14, 15, 16] As these children grow older and the deformity recurs, guided growth or supracondylar femoral osteotomy may be warranted. Patellar realignment may be necessary in some patients, and postoperative bracing and physical therapy may be indicated. The goal is to gain full extension and facilitate standing and walking.
The children with neurogenic FKFD will be considered together, acknowledging that spasticity management for cerebral palsy and spinal cord detethering for spina bifida may play an important role. For younger children, hamstring stretching, physical therapy, and bracing are useful temporizing measures. However, with growth, there may be inexorable progression of a crouch gait due to the insidious evolution of FKFD. When the fixed deformity surpasses 10º, most patients start to manifest symptoms such as fatigue, pain, or brace intolerance; these symptoms escalate at greater than 20 º. The energy costs of walking increase as the endurance and velocity decrease.[17, 18]
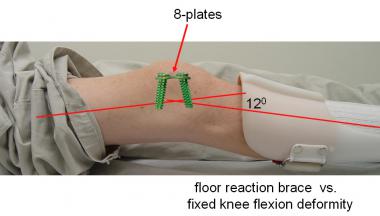 The efficacy of floor reaction braces is compromised in the presence of FKFD. However, they may be continued following guided growth, pending correction, whereupon bracing may be unnecessary, provided the quadriceps are sufficiently strong.
The efficacy of floor reaction braces is compromised in the presence of FKFD. However, they may be continued following guided growth, pending correction, whereupon bracing may be unnecessary, provided the quadriceps are sufficiently strong.
The indications and techniques for supracondylar osteotomy of the femur have been well described in standard textbooks and journals. Opinions vary as to whether internal or external fixation is preferable. In addition to the known risks of fixation failure, overcorrection or undercorrection, fracture, neurovascular compromise, skin slough, and recurrent deformity are very common.
There are specific situations in which the best option is gradual distraction and extension employing an external fixator[19] This may best serve those patients who have neglected or teratologic deformities, such as pterygium syndrome, or have reached skeletal maturity. Despite the touted advantages, it is a costly and slow process that usually requires a posterior release and that may not be well tolerated by the patient. Unfortunately, there is an acknowledged high rate of recurrent deformity despite postoperative bracing.
The distal femoral physis grows fairly rapidly, even in this population. Furthermore, skeletal maturity may be delayed, extending the window of opportunity for gradually straightening the knee by means of distal anterior femoral hemiepiphysiodesis. This may be safely undertaken even in relatively young children, without causing permanent growth arrest.[19, 20] Formerly accomplished with staples, the rate of correction has been improved by using 8-plates (Orthofix) — one placed on each side of the patellofemoral sulcus.
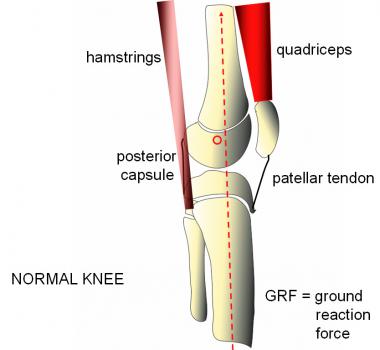 Normal sagittal alignment permits the knee to lock in full extension, aided by powerful quadriceps and an intact extensor mechanism. The ground reaction force passes anterior to the "center of rotation" of the knee, while the PCL, posterior capsule, hamstrings, and gastrocnemius provide a tension band effect.
Normal sagittal alignment permits the knee to lock in full extension, aided by powerful quadriceps and an intact extensor mechanism. The ground reaction force passes anterior to the "center of rotation" of the knee, while the PCL, posterior capsule, hamstrings, and gastrocnemius provide a tension band effect.
See the list below:
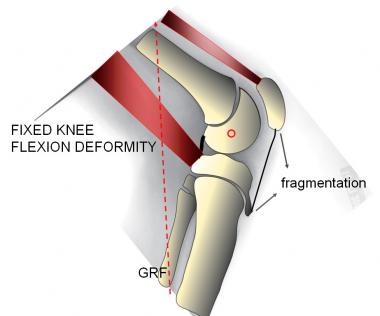 Fixed knee flexion deformity (FKFD). The knee is chronically bent, obligating the patient to walk with a crouch gait. The ground reaction force passes posterior to the center of rotation of the knee, where it overcomes the resistance of the weakened extensor mechanism. Secondary effects, including patella alta and fragmentation, are relatively common and painful.
Fixed knee flexion deformity (FKFD). The knee is chronically bent, obligating the patient to walk with a crouch gait. The ground reaction force passes posterior to the center of rotation of the knee, where it overcomes the resistance of the weakened extensor mechanism. Secondary effects, including patella alta and fragmentation, are relatively common and painful.
See the list below:
See the list below:
There are few contraindications to surgical correction of fixed knee flexion deformity (FKFD).
See the list below:
See the list below:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved