

Injuries to the flexor tendons of the hand are common. Each specific movement of the hand relies on the finely tuned biomechanical interplay of intrinsic and extrinsic musculotendinous forces. Considering the hand's role in labor, entertainment, art, literature, and passion, hand surgeons should fully define the normal and pathologic boundaries in each patient examined. With injuries that involve flexor tendons, fully defining the pathology is especially important.
In this article, management of flexor tendon injuries is addressed specifically, with emphases on history, physical examination, surgical repair, and rehabilitation.[1]
For patient education resources, see Hand Injuries and Finger Injuries.
NextFlexor tendons can become disrupted from either open or closed injuries. Minor puncture wounds or lacerations over the flexor tendon can result in partial or complete transection. Open injuries are often associated with other neurovascular deficits.
Closed injuries are frequently related to forced extension during active flexion of the finger. This type of avulsion injury, in which the flexor digitorum profundus (FDP) tendon ruptures at its insertion to the distal phalanx, is called Jersey finger. Flexor tendon rupture from chronic attrition may occur in rheumatoid diseases, Kienböck disease, scaphoid nonunion, a hamate fracture, or a Colles fracture.
The functional biomechanics of the flexor tendons depend on a number of factors, including an intact pulley system, synovial fluid, supple joints, and tendon excursion. The synovial fluid not only provides nutrients to the tendons but also is a constant source of lubrication, permitting frictionless gliding between the tendons. Adhesions between the tendons and other tissues restrict excursion. Stiff joints limit motion and function despite a normal tendon system.
The loss of the pulley system no longer prevents the tendons from gliding juxtaposed to the phalanges. The tendons bowstring away from the skeleton as the finger is flexed. This bowstringing increases the moment arm (a line drawn from the midaxis of the joint to the flexor tendon) of the tendon at that point. Greater excursion of the tendon and a greater amplitude of muscle contraction are required to obtain the same amount of finger flexion.
The clinical ramifications of tendon bowstringing are a weakened grip, incomplete flexion, and an ensuing stiffness of the joints. During normal tendon excursion, passive metacarpophalangeal (MCP) joint movement produces no relative motion of the flexor tendons. Distal interphalangeal (DIP) joint motion is 1-2 mm of FDP tendon excursion per 10 º of joint flexion. Proximal interphalangeal (PIP) joint motion is 1-2 mm of FDP tendon and flexor digitorum superficialis (FDS) tendon excursion per 10 º of joint flexion.
Differential excursion is increased with a palmar bar or synergistic splints (wrist extension). The overall excursion of the FDS and FDP tendons is approximately 88 mm and 86 mm, respectively, to obtain total digit and composite flexion. Excursion of 2.5 cm is required for complete flexion of the fingers.
Treatment and hand rehabilitation are based on the understanding of the tendon-injury healing mechanism. Healing of the flexor tendon system takes place in the following four stages or phases:
Hemostasis is characterized by vasoconstriction, platelet deposition, and fibrin clot. The amount of clot may affect the ultimate repair by increasing the number of adhesions.
Inflammation involves diapedesis of proinflammatory cells. Neutrophils and macrophages pass from the intravascular space to the extravascular space, proinflammatory cytokines are released, and fibronectin is used as scaffolding for collagen deposition and vascular ingrowth. This phase lasts approximately 0-7 days.
Proliferation is characterized by a marked rise in fibroblast proliferation occurring within 1 cm of the repair site. This phase lasts 2-28 days. The epitenon cells proliferate and migrate into the zone of injury. These cells are analogous to the epithelium of the skin, as they quickly cover the surface of the repair site in an attempt to restore a gliding surface. Collagen deposition rises markedly and rapidly as the fibroblasts proliferate. The vascular ingrowth can then migrate in via the collagen-fibronectin scaffolding.
Remodeling is marked by the growing strength of the repair. Collagen fibers are increasingly reoriented to become parallel with the noninjured tendon fibers, and collagen synthesis slows. The clinical importance of this phase, which starts at about week 6, is that during this interval, active and passive range of motion (ROM) is mandated to promote tendon excursion and diminish local adhesions. The ROM of all digits is increased, external scar control and blocking exercises are initiated, and resting exercises and strengthening procedures can be started.
Careful attention to the patient's history and the mechanism of injury can often alert the hand surgeon to the extent of the pathology.[2] Finger position at the time of injury is important. If the injury occurred while the finger was in flexion, the level of the tendon injury will be distal to the skin laceration. A finger that is injured in the extended position will have a tendon injury that closely corresponds to the skin laceration.
The natural resting position of the hand should be closely observed to determine whether the normal composite cascade of the fingers has been disrupted.
In the uninjured hand, the composite flexion of the fingers increases from the radial to the ulnar side. The finger with a tendon disruption nests in a more extended position. If only the FDP tendon has been transected, the flexion of the MCP and PIP joints may be within the normal cascade, but the DIP will be extended. A finger in which the FDS tendon and the FDP tendon are disrupted will lie flat in an extended position outside the normal cascade of fingers.
A thorough, formal examination of the FDS and FDP tendons is important because testing these tendons may reveal partial lacerations. A partial laceration may present with pain when the patient attempts to flex against resistance. A thorough neurovascular examination is warranted to alert the surgeon to the possible need for microsurgical repair of the vessels or nerves.[3]
The integrity of FDS and FDP tendons should be tested independently and in tandem. The examiner holds the other fingers in extension and stabilizes the MCP and PIP joints. To test the FDP tendon, the patient flexes the distal phalanx. To test the FDS tendon, MCP and PIP joints are released, distal phalanges are kept extended, and the patient flexes the finger. The PIP joint and, to a lesser degree, the MCP joint should flex. About 20% of patients are missing an FDS tendon in the little finger and thus have limited or no PIP flexion during testing.
For flexor pollicis longus (FPL) testing, the thumb MCP joint is stabilized in neutral position. The patient is asked to flex the interphalangeal (IP) joint against resistance. A communication may exist between the FPL and the index FDP. The examiner stabilizes the other three digits. The patient opposes his or her thumb to the little finger MCP joint. Flexion of the index distal phalanx proves the existence of this anomalous communication.
Two additional ways exist to evaluate the integrity of the flexor tendon. Passively manipulating the wrist through flexion and extension results in extension and flexion of the digits, respectively. This test uses the tenodesis effect of the antagonistic tendons. Compression of the forearm flexion muscles also can be used to test the integrity of the flexor tendons in the hand. As the forearm is compressed, the digits are drawn into flexion. Transected tendons in the digits do not flex with this maneuver, nor do they extend and flex with the tenodesis test.
Flexor tendons of the forearm originate from the muscles based on the medial epicondyle and on the proximal radius and ulna. Flexor tendon muscle bellies have three layers: superficial, intermediate, and deep.
The superficial layer consists of the pronator teres, which is the most radial of the superficial muscles. The flexor carpi radialis, palmaris longus, and flexor carpi ulnaris proceed in a radial-to-ulnar direction, respectively.
The FDS is the only muscle of the intermediate layer. This muscle has two separate heads of origin: the radial head of the medial epicondyle and the ulnar head of the ulna and radial head from the brief muscular line of the radius.
The two muscles of the deep layer are the FDP and the FPL. The FDP originates from the proximal two thirds of the ulna and from the interosseous membrane, and some element of the muscle may originate from the proximal radius. The FPL originates from the middle third of the radius and from the interosseous membrane.
The FDS and FDP tendons travel through the carpal tunnel to insert in the fingers. The FPL is the most radial structure of the radial tunnel; it extends on the volar aspect of the first ray. The FDP tendon inserts into the base of the distal phalanx, whereas the FDS tendon inserts into the base of the proximal phalanx. At the level of the A1 pulley, the FDS tendon decussates to form the Camper chiasma. The FDP tendon extends through the chiasma from below the FDS tendon to become the more superficial tendon.
The FDP tendon flexes the distal phalanx and secondarily flexes the PIP joint and the MCP joint; the FDS tendon flexes the PIP joint and secondarily flexes the MCP joint (see the image below).
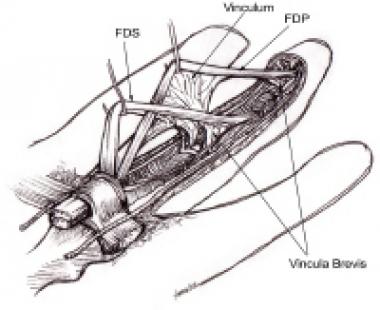 Flexor tendons with attached vincula.
Flexor tendons with attached vincula.
The ulnar nerve supplies the flexor carpi ulnaris, the ulnar two FDP tendons (to the little and ring fingers), and the intrinsic muscles of the hand (except for the radial two lumbrical muscles, the opponens pollicis, and the abductor pollicis brevis). The median nerve supplies the remaining extrinsic flexors in the forearm, the radial two lumbrical muscles, and the thenar muscles (except for the deep head of the flexor pollicis brevis [FPB], which is innervated by the ulnar nerve).
The fibro-osseous canal is the tunnel in the digits where the flexor tendons are located. The metacarpals form the dorsal wall, and the annular pulley system and flexor sheath provide radial, ulnar, and volar coverage. The flexor synovial sheath of the fingers is present from the midpalm up to the level of the FDP insertion. The sheath for the thumb and index finger often proceeds down through the carpal tunnel and can join up in the distal forearm in a horseshoe bursa configuration.
The annular and cruciform pulleys form an intricate constraining sheath to keep the tendons close to the bone, preventing bowstringing during their excursion to flex the MCP, PIP, and DIP joints. Three cruciform pulleys (C1-C3) and five annular pulleys (A1-A5) exist (see the image below). From a biomechanical vantage point, the A2 and A4 pulleys are considered the most important to the prevention of bowstringing.
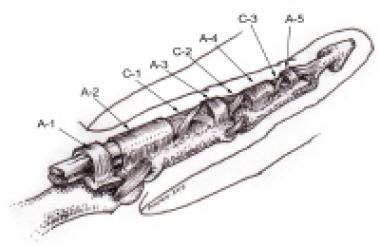 Retinacular portion of flexor tendon sheath.
Retinacular portion of flexor tendon sheath.
Flexor tendons have five different zones in the hand, as follows:
Nutrition to the tendons is derived from two sources: intrinsic and extrinsic. Intrinsic nutrition occurs through vascular perfusion of the tendon. The four sources of vascular perfusion are as follows:
The internal vascularity of the tendon is primarily positioned in the septa of the endotendon separating the tendon fascicles. It should be noted that the vascular supply is mainly on the dorsal side of the tendons. The tendon in the area of the proximal phalanx also has a relatively poor blood supply. Extrinsic nutrition is provided by synovial fluid diffusion that occurs as synovial fluid is pumped into the tendon fibers during flexion and extension of the fingers.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved