

Nonarticular rheumatic pain syndromes can be classified into five general categories, as follows:
The more generalized and chronic the syndrome, the more difficult it is to treat.
The spectrum of nonarticular pain syndromes and their interactions with mood disorders and chronic fatigue is depicted in the image below. Comorbidity is common.[1, 2]
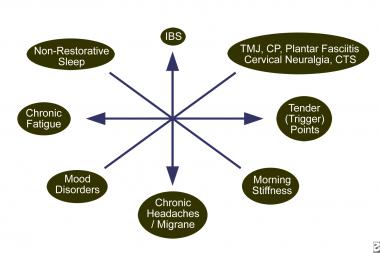 The spectrum of nonarticular myofascial pain syndromes.
The spectrum of nonarticular myofascial pain syndromes.
Next
Tendonitis presents as local pain, inflammation, dysfunction, and degeneration. It can be associated with overuse, infection, systemic rheumatic disease, or metabolic disturbance such as calcium apatite or pyrophosphate deposition. Fluoroquinolone antibiotic use can be associated with tendonitis and rupture. Inflammation can cause "triggering," in which the digit locks and a snapping sensation is felt upon release.[3]
Bursitis presents as local pain and inflammation of the synovial fluid filled saclike structures that protect soft tissues from underlying bone. Overuse, infection, systemic rheumatic disease, and metabolic disturbance such as calcium apatite and pyrophosphate deposition can also cause bursitis. Gout often causes olecranon bursitis and prepatellar bursitis.
Structural disorders such as scoliosis, lateral patellar subluxation, and flatfoot can cause local pain but are not always a source of pain or dysfunction.[4] The hypermobility syndrome presents with arthralgias due to increased joint laxity in the face of muscle disuse.
Neurovascular entrapment can occur centrally (eg, in spinal stenosis), in deep tissues (eg, thoracic outlet syndrome), or peripherally (eg, carpal or tarsal tunnel syndromes).[5, 6, 7, 8] Bone enlargement due to osteophytes, muscular tension, and inflammation can contribute to narrowing of a neurovascular passage. Pain and paresthesia usually occur distal to the site of entrapment.
Regional myofascial pain syndromes, such as temporomandibular joint syndrome, may represent a pain-spasm pain cycle triggered by mechanical injury, such as strain or overuse.[9]
Multiple bursitis and tendonitis syndrome present with anatomically localized areas of pain and dysfunction. Pain can be widespread, but the muscle tender points observed in fibromyalgia are absent. Usually, much less fatigue occurs, and responses to local therapies are better than in fibromyalgia.
Fibromyalgia, in many cases, presents as a form of allodynia, in which usually painless stimuli are perceived as painful, and hyperalgesia, in which normally painful stimuli is amplified. Cerebrospinal fluid levels of substance P are elevated, and additional abnormalities in the serotonin system and in the regulation of cortisol exist. Fibromyalgia can also coexist with various autoimmune diseases and often presents after a severe flulike syndrome, a defined infection (eg, Lyme disease), or trauma. Sleep is often disturbed, and nonrestorative sleep is associated with increased pain. The increased prevalence in females may point to a hormonal influence. Few abnormalities occur in the peripheral musculature. Studies that show abnormalities of cerebral blood flow in the thalamus and caudate nucleus help support the likelihood that pain processing in the central nervous system behaves abnormally.[10, 11, 12]
A recent study found that patients with fibromyalgia have an increased expression of sensory, adrenergic, and immune genes during moderate exercise.[13] Abnormalities of the neuroendocrine immune system are well documented, but none has yet been proven to be sensitive and specific enough to be used as a criterion for diagnosis.
Psychological, personality, and social factors may play important roles in many chronic cases of local and generalized pain syndromes. The image below depicts possible factors that contribute to the generation of these syndromes.
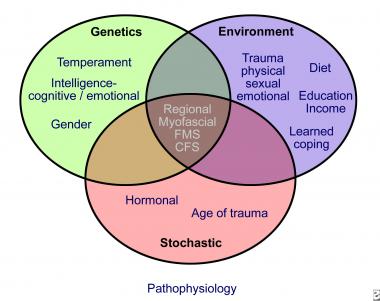 Possible factors that lead to myofascial pain syndromes.
Possible factors that lead to myofascial pain syndromes.
United States
The incidence of all types of soft tissue rheumatism has been estimated at about 4000 per 100,000 population. The prevalence rate of fibromyalgia is about 2% of the population.[14]
International
International incidence and prevalence are similar to those in the United States.
These syndromes are not life threatening but can be a cause of significant functional disability.[15, 16]
Racial differences in prevalence have not been reported.
Localized nonarticular rheumatism occurs with fairly equal distribution between males and females.
The female-to-male ratio of fibromyalgia is about 8:1, affecting about 3.5% of females and 0.5% of males in the United States.
Nonarticular rheumatism is most common in persons aged 45-64 years, and less than 0.2% of people with nonarticular rheumatism are younger than 14 years.
Fibromyalgia is most common in women in their fifth decade of life and is rare in prepubescent girls. The prevalence of fibromyalgia in women aged 60-79 years is 7%.[14, 16]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved