

Coxa vara includes all forms of decrease of the femoral neck shaft angle to less than 120-135°. Abnormal development of the proximal femoral cartilaginous physis and defective ossification of the adjacent metaphysis are responsible for the progressive decrease of the neck shaft angle. In severe cases, a separate triangular fragment involving the inferior-medial aspect of the femoral neck may also be found.
These anatomic and biologic factors underlying the biomechanical loading characteristics of the varus hip lead to a progressive inclination of the proximal epiphyseal plate, with shortening of the femoral neck and concomitant relative trochanteric overgrowth. A serious hip deformity, both clinically and radiographically, often results, for which the course is not always clear and the treatment is not always successful.
Coxa vara has many etiologies: congenital, acquired, and developmental. Congenital coxa vara (CCV), also referred to as infantile or cervical coxa vara, is a condition in which a varus deformity exists that is assumed to be caused by either an embryonic limb bud abnormality or an intrauterine condition causing significant proximal femoral varus. CCV is, by definition, present at birth but manifests clinically during early childhood and commonly follows a clinical course that is progressive with growth.[1, 2]
As a specific entity, CCV has characteristic clinical and radiographic features that help differentiate it from other forms of coxa vara. It is commonly associated with a significant limb-length discrepancy, segmental shortening of the femur, or other abnormalities of the bony femur. Associated diagnoses include proximal femoral focal deficiency (PFFD), congenital short femur, and congenital bowed femur.
Acquired forms of coxa vara are varus deformities of the proximal femur that develop secondary to metabolic, neoplastic, or traumatic conditions. This group includes ricketic coxa vara, fibrous dysplasia, proximal physeal injury, and premature closure. Also included in this category are secondary varus changes due to generalized skeletal conditions or dysplasias such as Morquio disease (mucopolysaccharidosis type IV), cleidocranial dysostosis, metaphyseal diaphyseal dysplasia, and metaphyseal dysostosis.
Fiorani first clinically described CCV in 1881.[3] Hofmeister, in 1894, first coined the term coxa vara and was the first to show radiographic evidence of a decreased neck shaft angle.[4] In 1905, Hoffa was the first to report on the histologic changes associated with coxa vara, and in 1928, Fairbank described the progressive tendency of the proximal femoral deformity during growth in coxa vara observed in childhood.[5, 6]
Duncan proposed in 1938 that progressive childhood coxa vara represented a deformity that appeared during the early years of growth, rather than being congenital, thus coining the term developmental coxa vara.[7] This proposal, although not generally accepted initially, was supported by the work of Amstutz in 1970.[8] Amstutz documented two patients who had normal findings on radiographs of the hips at birth but had radiographic evidence of coxa vara by age 2-3 years.
NextHistologic investigations by Chung and Riser and by Bos et al showed abnormalities in the proximal femoral physeal chondrocyte maturation, with disruption of the normal columnar architecture and abnormal calcification of the cartilaginous matrix.[9, 10] This abnormal enchondral ossification results in decreased production of metaphyseal bone, leading to a relative osteoporosis and subsequent weakness in this area. Notably, no evidence exists in these studies or others of an avascular-type process or of any pathologic or radiologic signs suggesting slippage of the proximal physeal plate as an underlying cause of the observed coxa vara.
Biomechanically, the sheer effect causing progressive varus deformity is best understood in relation to the resultant force (R) at the femoral/acetabular articulation (see the image below).[11] In the normal hip, this resultant force is perpendicular and compressive (C) in nature with respect to the physis. The force transmitted to the proximal femoral neck includes a net tension force (T) at the superior or lateral cortex and a net compressive force (C) at the inferior or medial cortex.
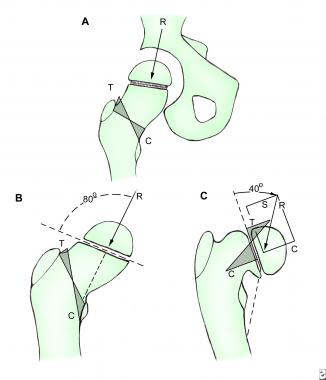 Congenital coxa vara (CCV). Hip biomechanics in coxa vara. (A, B) Normal hip. (C) Abnormal varus hip. Biomechanically, the sheer effect causing progressive varus deformity is best understood in relation to the resultant force (R) at the femoral/acetabular articulation. In the normal hip, this resultant force would be perpendicular and compressive (C) in nature with respect to the physis. The force transmitted to the proximal femoral neck would include a net tension force (T) at the superior or lateral cortex and a net compressive force (C) at the inferior or medial cortex. In the case of CCV, the more vertical position of the proximal femoral physis would increase not only the sheer component (S) of the hip articulation resultant force but also the net medial compressive force (C) on the metaphyseal bone of the femoral neck. These forces overwhelm the mechanical strength of the abnormally ossified bone in this area. This may lead to a relentless and progressive cycle of deformity that oftencontinues unless these forces are corrected with surgical intervention.
Congenital coxa vara (CCV). Hip biomechanics in coxa vara. (A, B) Normal hip. (C) Abnormal varus hip. Biomechanically, the sheer effect causing progressive varus deformity is best understood in relation to the resultant force (R) at the femoral/acetabular articulation. In the normal hip, this resultant force would be perpendicular and compressive (C) in nature with respect to the physis. The force transmitted to the proximal femoral neck would include a net tension force (T) at the superior or lateral cortex and a net compressive force (C) at the inferior or medial cortex. In the case of CCV, the more vertical position of the proximal femoral physis would increase not only the sheer component (S) of the hip articulation resultant force but also the net medial compressive force (C) on the metaphyseal bone of the femoral neck. These forces overwhelm the mechanical strength of the abnormally ossified bone in this area. This may lead to a relentless and progressive cycle of deformity that oftencontinues unless these forces are corrected with surgical intervention.
In the case of CCV, the more vertical position of the proximal femoral physis increases not only the sheer component (S) of the hip articulation resultant force, but also the net medial compressive force (C) on the metaphyseal bone of the femoral neck. These forces overwhelm the mechanical strength of the abnormally ossified bone in this area. This may lead to a relentless and progressive cycle of deformity that continues unless these forces are corrected with surgical intervention.
A few studies in the literature have described CCV as a variant of a chronic slip, with the continued varus biomechanically predisposing to increased shear stresses across the proximal femoral physis. The changes found in the cartilage of this physis are suggested to resemble those found in slipped capital femoral epiphysis (SCFE).
Other studies suggest that imaging (eg, magnetic resonance imaging [MRI]) results are not similar to those of SCFE and that a chronic slip theory does not explain the bone changes found in the metaphyseal bone of the proximal femur. The authors believe that a more generalized bone abnormality is present that predisposes these patients to deformity. Future investigations may shed further light on this topic.
The exact cause of CCV remains unknown. Many hypotheses have been proposed, including the following: mechanical intrauterine stresses affecting hip development; avascular necrosis involving selected areas of the proximal femoral physis/head and neck; and metabolic abnormalities causing deficient production of, or a delay in, the normal ossification process of the proximal end of the femur.
DiFazio et al reported on four patients with coxa vara who had neonatal extracorporeal membrane oxygenation (ECMO).[12]
Pylkkanen proposed what remains the most widely accepted theory on the cause of CCV.[13] He postulated that the proximal femoral deformity is the result of a primary ossification defect in the inferior femoral neck, on which physiologic shearing stresses (applied during weightbearing) cause fatigue of the local dystrophic bone, resulting in progressive varus deformity.
CCV is believed to be a relatively rare condition, with a reported incidence ranging from 1 per 13,000 population to 1 per 25,000 population. Relative to developmental dysplasia of the hip (DDH), it is estimated to occur less frequently, with the CCV-to-DDH ratio ranging from 1:13 to 1:20. No clear pattern of inheritance has been elucidated, but familial involvement in a number of cases has suggested an autosomal dominant genetic pattern of transmission.
No sex predilection appears to exist, and reported rates of right- and left-side involvement are essentially equal. Bilateral involvement seems to occur only half as often as unilateral involvement. Although some authors propose that no racial predilection exists, there is some suggestion that incidence is higher in persons of African descent than in whites.
Serafin and Szulc retrospectively reviewed 130 hips with CCV (mean follow-up, ~9 years).[14] The indication for surgery was a neck shaft angle of less than 110°, and they suggested correction of the Hilgenreiner epiphyseal angle (HEA) to less than 35-40°. Surgical treatment yielded good results in 80% of 2- to 9-year-olds, 62% in 10- to 11-year-olds, and 52% in 12- to 16-year-olds. Growth disturbances noted were a decrease in femoral head size (87%), flattening (43%), shallowness and underdevelopment of the acetabulum (76%), and shortening of the femoral neck. The authors suggested that most of these changes were reversible to some extent if surgical correction was undertaken in children aged 2-9 years.
Desai and Johnson reported their experience with valgus subtrochanteric osteotomies in 20 hips.[15] Age of patient at evaluation averaged 7 years, with surgery at an average age of 8 years and 20-year follow-up. Preoperative HEAs averaged 66°, and postoperative HEAs averaged 30°. Five also had greater trochanteric apophysiodesis at the discretion of the surgeon.
Good radiographic outcomes were noted in 89% of these patients, with Iowa hip scores of more than 90 points in all but one patient.[15] They reported a recurrence rate of 16%, citing inadequate correction (mean HEA >43°), and there was eventual healing with repeat osteotomies. Trochanteric overgrowth was noted in 63% of their patients, and adductor weakness was noted in 41%. No patients had a limb-length discrepancy of more than 2 cm, though two had undergone epiphysiodesis prior to maturity with projected discrepancies of 2 cm and 4.2 cm respectively.
Weinstein et al reviewed 20 patients with 25 hips affected with CCV.[16] Average age at diagnosis was 5.75 years, age at treatment averaged 6.6 years, and mean follow-up was 15.3 years. Average HEA preoperatively measured 82.1°, and the preoperative mean head-shaft angle was 89.9°, corrected to 132.4°. Postoperative HEAs were not reported.
The authors noted that 85.3% of initial correction was maintained at final follow-up.[16] In patients older than 5 years at the time of surgery, 75% maintained better than 80% correction, whereas in patients younger than 5 years, only 37% maintained 80% correction or better. A possible reason for this rate of correction, as well as whether it was related to greater trochanteric overgrowth, expected to be more of an issue in the younger patient, was not elucidated. This was the landmark article introducing the concept of the HEA as a predictor of progression in developmental coxa vara.
As with any treatment, long-term results remain the mainstay of evaluation of utility and effectiveness. Available long-term evaluations of CCV show that with the proper diagnosis and indications for surgery and, most importantly, adequate correction of the deformity of the proximal femur, an optimistic outlook can be adopted for most patients affected by this condition.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved