

Deltoid fibrosis is a disorder marked by intramuscular fibrous bands within the substance of the deltoid muscle. These bands lead to secondary contractures that affect the function of the shoulder joint.[1] Scapular winging and secondary scoliosis may also be related to this condition.[2] Similar contractures have also been seen in the quadriceps and gluteal muscles.[3, 4] Some patients exhibit contractures in both the upper and lower extremities.
Deltoid fibrosis is part of a spectrum of fibrotic conditions that affect both upper and lower extremities. Such fibrotic conditions may involve one extremity or, in rare cases, all four. Contracture of a muscle may limit limb mobility, leading to a decrease in function and an abnormal appearance, which, in turn, may have social implications. Deltoid fibrosis is seen in people of all ages, but it has been reported primarily in children. Most frequently, affected individuals cannot bring their arm down to touch the side of their body. They may also exhibit a winging (pulling backwards) of the scapula.
Significant documentation of deltoid fibrosis began in the early 1960s. Isolated reports of the condition had been made before then, but not in the English-language medical literature. After World War II, parenteral administration of antibiotics, antipyretics, and other drugs became increasingly common. Along with the increased use of intramuscular injections came the appearance of deltoid fibrosis and contractures, as well as problems in other muscle groups. It is believed that these repeated procedures disrupt the anatomic features in the area of the injection.
Deltoid fibrosis is an uncommon problem. In children, it may be related to congenital/developmental defects or to intramuscular injections. Patients who develop contractures following injection likely have an inherent genetic predisposition for the development of fibrosis. In adults, contractures seem to be related to injection frequency. In Japan, Ogawa reported that with the exception of a few adult cases, no new cases of deltoid contracture have been documented since the risks of intramuscular injection were publicized in 1975. Therefore, with the exception of a few isolated cases, deltoid fibrosis may become a problem of historical interest.
NextThe deltoid muscle (see the image below) has three areas of origin: the clavicle, the acromion, and the scapular spine. There is one site of insertion, the deltoid tubercle on the humerus.
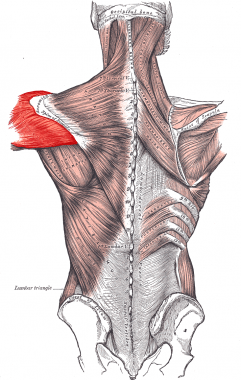 Deltoid muscle.
Deltoid muscle.
The deltoid muscle is divided into three portions: anterior, middle, and posterior. The anterior and posterior portions converge directly into the insertion site, whereas the middle portion has multiple branches leading to a central tendon. The middle portion has four intramuscular septa that extend distally from the lateral acromion and interdigitate with three septa that insert on the deltoid tubercle.
The main action of the deltoid is abduction of the arm. The anterior deltoid also assists in forward flexion and internal rotation. The posterior portion assists with extension and external rotation.
Contractures of the deltoid have been reported in all three portions of the muscle but are seen most commonly in the middle portion. The second most common site for contracture is the posterior portion. It is thought that these areas are involved most commonly because injections are placed there to avoid the cephalic vein anteriorly, although anterior bands are occasionally seen. Two portions, or even all three portions, have been reported to be involved with contracture.[3, 5, 6, 7, 8, 9, 10, 11]
Electromyography (EMG) findings have shown decreased-to-absent activity in the involved muscle, but nerve conduction studies have been normal. Chen et al showed that EMG abnormalities are observed not only in the involved muscle but also in the uninvolved adjacent muscles.[12, 13] This suggests that the muscle is abnormal initially and is especially susceptible to injury and the development of fibrosis. A diagnosis can be made from the findings of fibrous cords on magnetic resonance imaging (MRI) of the deltoid muscle.[14]
Chen et al proposed the following three possible mechanisms for the development of deltoid contractures[12] :
Repeated injection injuries, myotoxicity, or both are believed to trigger fibrotic deltoid contracture by causing focal myositis and subsequent myopathic degeneration. Denervation occurs simultaneously from fibrotic compression or ischemia. It is also likely that injury occurs in connective tissue as well as in muscle. This could be caused by an enzyme deficiency in collagen degradation, an increased rate of collagen synthesis, genetic defects in the regulation of collagen biosynthesis, or an enzymatic defect in fibroblasts.
Some or all of these factors are undoubtedly at work, independent of muscle injury, in that almost all series of deltoid fibrosis studies include some patients who do not have a history of deltoid injections. Hogendoorn et al reported on infants with brachial plexus injuries during birth.[15] These individuals experienced contracture of the arm with muscle paralysis. The lack of innervation to certain muscles led to overcompensation by nearby muscles, along with osseous deformities. Scott and Alexander described a patient with a deltoid contracture secondary to an osteochondroma of the scapula.[2]
Deltoid fibrosis has most commonly been related to intramuscular postinjection events, with trauma, congenital factors, and progressive idiopathic factors also playing roles.[16] Antibiotics, antipyretics, and other commonly injected medications seem to influence contractures of the deltoid.[17, 18]
Although these factors seem to play a leading role, the exact cause of fibrous development is unknown. Chen et al found that siblings of affected children had similar contractures in only 30% of cases,[12] despite a similar frequency of injections.
Development of deltoid fibrosis is not limited to children. Multiple cases have been reported of fibrosis development in older adults who received frequent injections. However, Manske reported findings of contractures in infants with no history of injections.[19] These children had been exposed only to physical trauma and birthing complications. Chatterjee and Gupta also examined multiple patients presenting with deltoid fibrosis that denied a significant history of intramuscular injections, indicating that other factors must be contributing to fibrosis formation.[5]
It has been reported that progressive systemic sclerosis can cause deltoid fibrosis as well as its hallmark cutaneous manifestations.[20] An association with hypertrophic scar formation and keloid formation has also been noted with muscular fibrosis and contracture.[6]
In certain areas of the world, specifically Asian countries, contractures have become more common. In Taiwan, the prevalence has reached 10% in some areas. This growing frequency is thought to be due to increased intramuscular injections as treatment for infections and fevers.[12, 21]
In the United States, the incidence of deltoid fibrosis has been low. Reports on small groups of patients with deltoid fibrosis have been made, but no large series have been reported in the United States. All of the large series on this condition are from abroad.
Several series have reported about a 6% incidence of recurrence. With distal release, Chen et al reported good outcomes in 100% of patients,[13] and Ko et al reported good range of motion and pain relief in 96% of patients following surgical release.[22]
Patients who had distal release were evaluated with a Cybex dynamometer and were found to have no loss of strength compared with the contralateral side. Function returned to normal within 3 months.[13]
In general, the degree of preoperative contracture does not correlate with postoperative results.[14] Whether the shoulder is treated with proximal or distal release, it appears that the rate of complications is low and that the great majority of patients see a return of full range of motion, excellent pain relief, and a resolution of scapular winging. The results of distal release are reported as equivalent to proximal release, leading most to believe that distal release should be considered routinely. Distal release avoids the stair-step deformity associated with a proximal release.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved