

During the past 50 years, the treatment of subtrochanteric fractures has evolved in conjunction with improved understanding of both fracture biology and biomechanics. Previously, nonsurgical treatment of these fractures was associated not only with significant shortening and malrotation but also with the morbidity and mortality of prolonged immobilization. Early surgical repair techniques had unacceptably high complication rates; however, the benefits of restoring the anatomy and encouraging early mobilization are recognized and have led to significant research and improvement in implants. Currently, subtrochanteric fractures remain technically challenging, even to experienced fracture surgeons.[1, 2]
The difficulty of treating these fractures stems in part from the fact that this injury pattern is anatomically distinct from other proximal femoral peritrochanteric fractures and in part from the difficult features of femoral shaft fractures. As a result, they must be treated with specially designed implants that can withstand significant muscular forces for prolonged periods of healing. These strong muscle forces deform the fracture fragments and make reduction difficult. In addition, comminution is common in this region, and implants must withstand significant early loading.
Not surprisingly, subtrochanteric fracture has significantly higher rates of malunion and nonunion than other femoral fractures. Still, with an improved understanding of this fracture and the specific treatment options, successful results can be obtained.[1, 2]
NextThe subtrochanteric region of the femur, arbitrarily designated as the region between the lesser trochanter and a point 5 cm distal, consists primarily of cortical bone. The femoral head and neck are anteverted approximately 13º with respect to the plane of the femoral shaft. The piriformis fossa lies at the base of the neck and is oriented in line with the femoral shaft. The lesser trochanter is posteromedial, and it is the point of insertion for the psoas and iliacus tendons. The femoral shaft has both an anterior and a lateral bow.
The major muscles that surround the hip create significant forces that contribute to fracture deformity. The gluteus medius and minimus tendons attach to the greater trochanter and abduct the proximal fragment. The psoas and iliacus attach to the lesser trochanter and flex the proximal fragment. The adductors pull the distal fragment medially.
All of these muscles are well vascularized, and this can lead to significant hemorrhage at the time of injury or during surgical approaches. To approach the proximal lateral femur, the vastus lateralis must be split or elevated off the intermuscular septum close to the large perforating branches of the profunda femoris. Division of these vessels can lead to copious bleeding, making surgical exposure difficult. With open surgical procedures, meticulous handling of these vessels and soft tissue is of paramount importance because the blood supply is critical to fracture healing.
The subtrochanteric region of the femur heals predominantly through a primary cortical healing; consequently, a subtrochanteric fracture is quite slow to consolidate.[3] In addition, this region is exposed to high stresses during activities of daily living. Axial loading forces through the hip joint create a large moment arm, with significant lateral tensile stresses and medial compressive loads.
The calcar is a portion of bone along the posteromedial femur, just below the lesser trochanter, that extends proximally into the posteroinferior femur. Significant compressive forces have been described in this region, which contribute to the dense cortical bone of the subtrochanteric femur. A man who weighs 200 lb can generate forces in excess of 1200 lb per square inch (psi).[4]
In addition to the bending forces, muscle forces at the hip also create torsional effects that lead to significant rotational shear forces. During normal activities of daily living, up to six times the body weight is transmitted across the subtrochanteric region of the femur.[5]
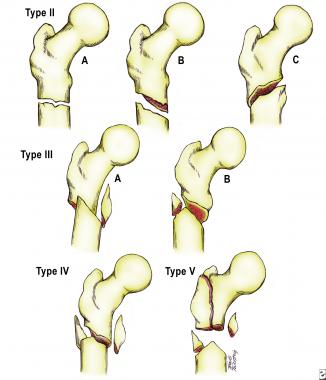
A universally accepted fracture classification does not exist for subtrochanteric femur fractures. The Arbeitsgemeinschaft für Osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) developed a complicated three-part classification system with 10 subtypes (see the image below); this system is most useful in research settings.
 The Arbeitsgemeinschaft für osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) classification of subtrochanteric femur fractures.
The Arbeitsgemeinschaft für osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) classification of subtrochanteric femur fractures.
In 1978, Seinsheimer presented an important classification with eight subgroups that identified fractures with loss of medial cortical stability (see the image below).[6]
 The Seinsheimer classification of subtrochanteric femur fractures.
The Seinsheimer classification of subtrochanteric femur fractures.
The Russell-Taylor classification system (see the image below) is helpful because it assists in determining the proper mode of treatment.
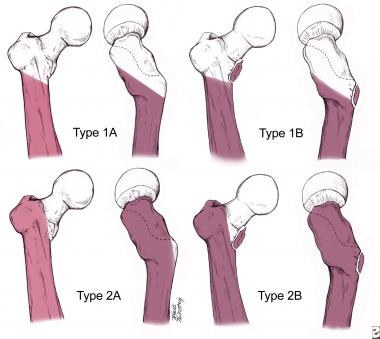 The Russell-Taylor classification of subtrochanteric femur fractures.
The Russell-Taylor classification of subtrochanteric femur fractures.
Russell-Taylor type 1 fractures do not involve the piriformis fossa. They are subdivided into subtypes A (for fractures below the lesser trochanter) and B (for fractures involving the lesser trochanter). Type 2 fractures involve the piriformis fossa. Type 2A fractures have a stable medial buttress. Type 2B has no stability of the medial femoral cortex. These fractures may have varying degrees of proximal comminution, sometimes with extension into the femoral neck, and may present difficulty with implant choice.
Type 1 fractures can be treated with first-generation or second-generation intramedullary devices. Historically, type 2 fractures were treated by means of open reduction and internal fixation (ORIF) with plate and screw devices or fixed-angle implants. With advanced techniques and implant design, intramedullary fixation has been a successful tool with reliable rates of healing.
In elderly patients, minor slips or falls that lead to direct lateral hip trauma are the most frequent mechanism of injury.[7, 8] This age group is also susceptible to metastatic disease that can lead to pathologic fractures. In younger patients, the mechanism of injury is almost always high-energy trauma, either from direct lateral trauma (eg, motor vehicle accident [MVA]) or from axial loading (eg, a fall from height).
Gunshot wounds cause approximately 10% of high-energy subtrochanteric femur fractures. Iatrogenic fractures may also occur secondary to stress risers following previous surgery on the proximal femur.[9]
Subtrochanteric fractures account for approximately 10-30% of all hip fractures, and they affect persons of all ages. Most frequently, these fractures are seen in two patient populations—namely, older osteopenic patients who have sustained a low-energy fall[8, 10] and younger patients who have been involved in high-energy trauma. A more recently identified patient population consists of individuals who experience subtrochanteric fractures after bisphosphonate use. These so-called atypical fractures have a transverse or short oblique pattern with cortical thickening and a medial cortical "beak."
Relatively few data exist regarding the outcome of patients with subtrochanteric femur fractures.[11] In young patients, these injuries are common among those with multiple traumatic injuries; thus, outcomes are likely to be poorer than those in patients with isolated femur fractures. Associated fractures and soft-tissue injuries to the knee can complicate rehabilitation efforts. In older patients, subtrochanteric fractures can be grouped with other proximal femur fractures with relatively high morbidity and mortality.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved